Uterine cancer: Difference between revisions
Changed image for thumbnail to make more approachable for patient viewing. |
tweak cites |
||
| (48 intermediate revisions by 22 users not shown) | |||
| Line 1: | Line 1: | ||
{{cs1 config|name-list-style=vanc|display-authors=6}} |
|||
{{Infobox medical condition (new) |
{{Infobox medical condition (new) |
||
| name = Uterine cancer |
| name = Uterine cancer |
||
| Line 14: | Line 15: | ||
| types = [[Endometrial cancer]], [[uterine sarcoma]]<ref name=NCI2019Pt/> |
| types = [[Endometrial cancer]], [[uterine sarcoma]]<ref name=NCI2019Pt/> |
||
| causes = |
| causes = |
||
| risks = '''Endometrial cancer''': [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], family history of the condition<ref name=NCI2019PtEndo/><br>'''Uterine sarcoma''': [[radiation therapy]] to the pelvis<ref name=NCI2019PtSar/> |
| risks = '''Endometrial cancer''': [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], tamoxifen use, unopposed estrogens, late menopause, family history of the condition<ref name=NCI2019PtEndo/><br>'''Uterine sarcoma''': [[radiation therapy]] to the pelvis<ref name=NCI2019PtSar/> |
||
| diagnosis = |
| diagnosis = |
||
| differential = |
| differential = |
||
| Line 24: | Line 25: | ||
}} |
}} |
||
<!-- Definition and symptoms --> |
<!-- Definition and symptoms --> |
||
'''Uterine cancer''', also known as '''womb cancer''', includes two types of [[cancer]] that develop from the tissues of the [[uterus]].<ref name=NCI2019Pt>{{cite web |title=Uterine Cancer |url=https://www.cancer.gov/types/uterine |website=National Cancer Institute |access-date=3 February 2019 |language=en |date=1 January 1980}}</ref> [[Endometrial cancer]] forms from the [[endometrium|lining of the uterus]], and [[uterine sarcoma]] forms from the muscles or support tissue of the uterus.<ref name=NCI2019PtEndo>{{cite web |title=Endometrial Cancer Treatment |url=https://www.cancer.gov/types/uterine/patient/endometrial-treatment-pdq#section/all |website=National Cancer Institute |access-date=3 February 2019 |language=en|date=26 April 2018}}</ref><ref name=NCI2019PtSar>{{cite web |title=Uterine Sarcoma Treatment |url=https://www.cancer.gov/types/uterine/patient/uterine-sarcoma-treatment-pdq#section/all |website=National Cancer Institute |access-date=3 February 2019 |language=en |date=3 October 2018}}</ref> Symptoms of endometrial cancer include changes in [[vaginal bleeding]] or pain in the [[pelvis]].<ref name=NCI2019PtEndo/> Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.<ref name=NCI2019PtSar/> |
'''Uterine cancer''', also known as '''womb cancer''', includes two types of [[cancer]] that develop from the tissues of the [[uterus]].<ref name=NCI2019Pt>{{cite web |title=Uterine Cancer |url=https://www.cancer.gov/types/uterine |website=National Cancer Institute |access-date=3 February 2019 |language=en |date=1 January 1980}}</ref> [[Endometrial cancer]] forms from the [[endometrium|lining of the uterus]], and [[uterine sarcoma]] forms from the muscles or support tissue of the uterus.<ref name=NCI2019PtEndo>{{cite web |title=Endometrial Cancer Treatment |url=https://www.cancer.gov/types/uterine/patient/endometrial-treatment-pdq#section/all |website=National Cancer Institute |access-date=3 February 2019 |language=en|date=26 April 2018}}</ref><ref name=NCI2019PtSar>{{cite web |title=Uterine Sarcoma Treatment |url=https://www.cancer.gov/types/uterine/patient/uterine-sarcoma-treatment-pdq#section/all |website=National Cancer Institute |access-date=3 February 2019 |language=en |date=3 October 2018}}</ref> Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States.<ref name="Felix 985–994">{{cite journal | vauthors = Felix AS, Brinton LA | title = Cancer Progress and Priorities: Uterine Cancer | journal = Cancer Epidemiology, Biomarkers & Prevention | volume = 27 | issue = 9 | pages = 985–994 | date = September 2018 | pmid = 30181320 | pmc = 6504985 | doi = 10.1158/1055-9965.EPI-18-0264 }}</ref> Symptoms of endometrial cancer include changes in [[vaginal bleeding]] or pain in the [[pelvis]].<ref name=NCI2019PtEndo/> Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the [[vagina]].<ref name=NCI2019PtSar/> |
||
<!-- Cause and risk factors --> |
<!-- Cause and risk factors --> |
||
Risk factors for endometrial cancer include [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], taking pills that contain estrogen without progesterone, a history of [[tamoxifen]] use, late menopause, and a family history of the condition.<ref name=" |
Risk factors for endometrial cancer include [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], taking [[Estrogen therapy|pills that contain estrogen without progesterone]], a history of [[tamoxifen]] use, late [[menopause]], and a family history of the condition.<ref name="www.cancer.org">{{Cite web|title=Endometrial Cancer Risk Factors|url=https://www.cancer.org/cancer/endometrial-cancer/causes-risks-prevention/risk-factors.html|access-date=2021-09-13|website=www.cancer.org|language=en}}</ref><ref name=NCI2019PtEndo/> Risk factors for uterine sarcoma include prior [[radiation therapy]] to the pelvis.<ref name=NCI2019PtSar/> Diagnosis of endometrial cancer is typically based on an [[endometrial biopsy]].<ref name=NCI2019PtEndo/> A diagnosis of uterine sarcoma may be suspected based on symptoms, a [[pelvic exam]], and [[medical imaging]].<ref name=NCI2019PtSar/> |
||
<!-- Treatment and prognosis --> |
<!-- Treatment and prognosis --> |
||
Endometrial cancer can often be cured while uterine sarcoma typically is harder to treat.<ref name=NCI2019Pt/> Treatment may include a combination of [[surgery]], [[radiation therapy]], [[chemotherapy]], [[hormone therapy]], and [[targeted therapy]].<ref name=NCI2019PtEndo/><ref name=NCI2019PtSar/> Just over 80% of |
Endometrial cancer can often be cured while uterine sarcoma typically is harder to treat.<ref name=NCI2019Pt/> Treatment may include a combination of [[surgery]], [[radiation therapy]], [[chemotherapy]], [[hormone therapy]], and [[targeted therapy]].<ref name=NCI2019PtEndo/><ref name=NCI2019PtSar/> Just over 80% of women survive more than 5 years following diagnosis.<ref name=SEER2019/> |
||
<!-- Epidemiology and culture --> |
<!-- Epidemiology and culture --> |
||
In 2015 about 3.8 million |
In 2015 about 3.8 million women were affected globally and it resulted in 90,000 deaths.<ref name=GBD2015Pre>{{cite journal | vauthors = | title = Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015 | journal = Lancet | volume = 388 | issue = 10053 | pages = 1545–1602 | date = October 2016 | pmid = 27733282 | pmc = 5055577 | doi = 10.1016/S0140-6736(16)31678-6 }}</ref><ref name=GBD2015De>{{cite journal | vauthors = | title = Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015 | journal = Lancet | volume = 388 | issue = 10053 | pages = 1459–1544 | date = October 2016 | pmid = 27733281 | pmc = 5388903 | doi = 10.1016/S0140-6736(16)31012-1 }}</ref> Endometrial cancer is relatively common while uterine sarcomas are rare.<ref name=NCI2019Pt/> In the United States, uterine cancers represent 3.5% of new cancer cases.<ref name=SEER2019>{{cite web |title=Uterine Cancer - Cancer Stat Facts |url=https://seer.cancer.gov/statfacts/html/corp.html |website=SEER |access-date=3 February 2019 |language=en}}</ref> They most commonly occur in women between the ages of 45 and 74 with a median age of diagnosis of 63.<ref name=SEER2019/> |
||
== Types == |
== Types == |
||
The terms uterine cancer and womb cancer may refer to |
The terms uterine cancer and womb cancer may refer to several different types of [[cancer]] that occur in the [[uterus]], namely: |
||
=== [[Endometrial cancer]] |
=== [[Endometrial cancer]] === |
||
* ''Endometrial carcinomas'' originate from cells in the glands of the [[endometrium]] (uterine lining). These include the common and readily treatable ''well-differentiated endometrioid adenocarcinoma,'' as well as the more aggressive ''[[Uterine serous carcinoma|uterine papillary serous carcinoma]]'' and ''[[uterine clear-cell carcinoma]]''.<ref name=" |
* ''Endometrial carcinomas'' originate from cells in the glands of the [[endometrium]] (uterine lining). These include the common and readily treatable ''well-differentiated endometrioid adenocarcinoma,'' as well as the more aggressive ''[[Uterine serous carcinoma|uterine papillary serous carcinoma]]'' and ''[[uterine clear-cell carcinoma]]''.<ref name="www.cancer.org_2">{{Cite web|title=What Is Endometrial Cancer?|url=https://www.cancer.org/cancer/endometrial-cancer/about/what-is-endometrial-cancer.html|access-date=2021-09-14|website=www.cancer.org|language=en}}</ref> |
||
* ''[[Mixed Müllerian tumor|Malignant mixed Müllerian tumors]]'' (also known as uterine carcinosarcomas) are rare endometrial tumors which show both glandular ([[carcinoma]]tous) and stromal ([[sarcoma]]tous) differentiation.<ref name=" |
* ''[[Mixed Müllerian tumor|Malignant mixed Müllerian tumors]]'' (also known as uterine carcinosarcomas) are rare endometrial tumors which show both glandular ([[carcinoma]]tous) and stromal ([[sarcoma]]tous) differentiation.<ref name="www.cancer.org_2" /> |
||
=== [[Uterine sarcoma]]s |
=== [[Uterine sarcoma]]s === |
||
*[[Leiomyosarcoma|''Leiomyosarcomas'']] originate from the muscular layer of the uterus (or [[myometrium]]). Of note, leiomyosarcomas are distinct from [[Uterine fibroid|uterine leiomyomas]], which are benign tumors of the uterus.<ref name=" |
*[[Leiomyosarcoma|''Leiomyosarcomas'']] originate from the muscular layer of the uterus (or [[myometrium]]). Of note, leiomyosarcomas are distinct from [[Uterine fibroid|uterine leiomyomas]], which are benign tumors of the uterus.<ref name="www.cancer.org_3">{{Cite web|title=What Is Uterine Sarcoma?|url=https://www.cancer.org/cancer/uterine-sarcoma/about/what-is-uterine-sarcoma.html|access-date=2021-09-14|website=www.cancer.org|language=en}}</ref> |
||
| ⚫ | |||
== Signs and symptoms == |
|||
| ⚫ | |||
Both types of uterine cancer can present with abnormal vaginal bleeding and discharge.<ref name="www.uptodate.com">{{Cite web|title=Endometrial carcinoma: Clinical features, diagnosis, prognosis, and screening|url=https://www.uptodate.com/contents/endometrial-carcinoma-clinical-features-diagnosis-prognosis-and-screening?search=uterine%20cancer&topicRef=16917&source=see_link|access-date=2021-09-18|website=www.uptodate.com}}</ref><ref name="www.uptodate.com_2">{{Cite web|title=Uterine sarcoma: Classification, epidemiology, clinical manifestations, and diagnosis|url=https://www.uptodate.com/contents/uterine-sarcoma-classification-epidemiology-clinical-manifestations-and-diagnosis?search=uterine%20sarcoma&source=search_result&selectedTitle=1~61&usage_type=default&display_rank=1|access-date=2021-09-18|website=www.uptodate.com}}</ref> Abnormalities can include change in duration or amount of menstrual bleeding as well as new bleeding between [[menses]] or after menopause. Sensations of new or increasing pelvic pressure or pain can also indicate tumor growth in the uterus.<ref name="www.uptodate.com_2" /> Any of these findings warrant further workup by a doctor. |
|||
== |
== Causes and risk factors == |
||
Both types of uterine cancer can present with abnormal vaginal bleeding and discharge. Abnormalities can include change in duration or amount of menstrual bleeding as well as new bleeding between menses or after menopause. Sensations of new or increasing pelvic pressure or pain can also indicate tumor growth in the uterus. Any of these warrant further workup by a doctor. |
|||
== Causes and Risk Factors == |
|||
<!-- Causes --> |
<!-- Causes --> |
||
It is not known with certainty what the causes for uterine cancer may be, though hormone imbalance is |
It is not known with certainty what the causes for uterine cancer may be, though hormone imbalance is cited as a risk factor. Estrogen receptors, known to be present on the surfaces of cells of this type of cancer, are thought to interact with the hormone causing increased cell growth, which can then result in cancer. The exact mechanism of how this occurs is not understood.<ref>[http://www.cancer.org/cancer/endometrialcancer/detailedguide/endometrial-uterine-cancer-what-causes Causes, Risk Factors, and Prevention TOPICS] - Do we know what causes endometrial cancer? - cancer.org - American Cancer Society - Retrieved 5 January 2015.</ref><!-- Risk factors --> |
||
Risk factors for endometrial cancer include [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], taking pills that contain estrogen without progesterone, a history of tamoxifen use, late menopause, and |
Risk factors for endometrial cancer include [[obesity]], [[metabolic syndrome]], [[type 2 diabetes]], taking pills that contain estrogen without progesterone, a history of [[tamoxifen]] use, late menopause, and certain hereditary conditions ([[Lynch Syndrome|Lynch syndrome]], [[Cowden syndrome]]).<ref name="www.cancer.org" /><ref name="NCI2019PtEndo" /><ref name="www.uptodate.com" /> Risk factors for uterine sarcoma include prior [[radiation therapy]] to the pelvis, a history of tamoxifen use, a history of childhood [[retinoblastoma]], and [[Hereditary leiomyomatosis and renal cell carcinoma|hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome]].<ref name="NCI2019PtSar" /><ref name="www.uptodate.com_2" /> |
||
== Diagnosis == |
== Diagnosis == |
||
To evaluate for uterine cancer, a clinician might perform a [[Pelvic examination|pelvic exam]] to visually inspect internal pelvic organs and to feel the size and position of the uterus and ovaries |
To evaluate for uterine cancer, a clinician might perform a [[Pelvic examination|pelvic exam]] to visually inspect internal pelvic organs and to feel the size and position of the uterus and ovaries. A “[[Pap test|pap smear]]” may also be done to brush the sides of the cervix to collect cells for testing and to look at under a microscope. A [[Dilation and curettage|dilatation and curettage]] is often done to collect a sample of uterine lining tissue. An [[Medical ultrasound|ultrasound]] is also often performed to look for tumors.<ref>{{Cite web|date=2012-06-25|title=Uterine Cancer - Diagnosis|url=https://www.cancer.net/cancer-types/uterine-cancer/diagnosis|access-date=2021-09-14|website=Cancer.Net|language=en}}</ref> |
||
== Screening and Prevention ==<!-- Screening --> |
== Screening and Prevention ==<!-- Screening --> |
||
Screening for uterine cancers is not recommended except for in |
Screening for uterine cancers is not recommended except for in women with certain hereditary conditions that increase their risk (Lynch, Cowden, HLRCC).<ref name="www.uptodate.com" /><ref name="www.uptodate.com_2" /> <!-- Prevention --> |
||
In general, [[ |
In general, [[combined oral contraceptive pill]]s and [[Progestogen-only pill|progestin-only pills]] are protective against uterine cancers. Weight loss and/or bariatric surgery reduces the risk for patients with obesity.<ref name="www.uptodate.com" /> |
||
== Treatment == |
== Treatment == |
||
Treatment of uterine cancer may differ depending on the type of cancer and staging of the tumor.<ref name=" |
Treatment of uterine cancer may differ depending on the type of cancer and staging of the tumor.<ref name="www.cancer.gov">{{Cite web|title=Uterine Cancer—Patient Version - National Cancer Institute|url=https://www.cancer.gov/types/uterine|access-date=2021-09-13|website=www.cancer.gov|language=en}}</ref> In early stages, minimal invasive surgery is preferred. <ref>{{cite journal | vauthors = Filippova OT, Leitao MM | title = The current clinical approach to newly diagnosed uterine cancer | journal = Expert Review of Anticancer Therapy | volume = 20 | issue = 7 | pages = 581–590 | date = July 2020 | pmid = 32531179 | pmc = 7416456 | doi = 10.1080/14737140.2020.1782750 }}</ref> |
||
For endometrial cancer, five main types of treatments are used, including surgery, [[radiation therapy]], [[chemotherapy]], hormone therapy, and targeted therapy. The most common treatment modality for endometrial cancer is surgery, whereby the uterus is removed via a total [[hysterectomy]].<ref name=" |
For endometrial cancer, five main types of treatments are used, including surgery, [[radiation therapy]], [[chemotherapy]], hormone therapy, and targeted therapy. The most common treatment modality for endometrial cancer is surgery, whereby the uterus is removed via a total [[hysterectomy]].<ref name="www.cancer.gov" /> Hysterectomies may also be accompanied by removal of ovaries and fallopian tubes, called a [[Salpingoophorectomy|salpingo-oophorectomy]]. Additionally, hormone therapy which seeks to block the growth of cancer cells may also be used in the treatment of endometrial cancer. Targeted therapy may include [[Monoclonal antibody|monoclonal antibodies]], [[mTOR inhibitors]], and [[Signal transduction inhibitor|signal transduction inhibitors]] which all act to target cancer cells specifically.<ref name="www.cancer.gov" /> |
||
As of 2021, treatment options for uterine sarcoma include surgery, radiation therapy, chemotherapy, and hormone therapy.<ref name=" |
As of 2021, treatment options for uterine sarcoma include surgery, radiation therapy, chemotherapy, and hormone therapy.<ref name="www.cancer.gov" /> |
||
== Prognosis == |
== Prognosis == |
||
[[Prognosis]] varies for the different types of endometrial cancer. Factors that influence prognosis across types of uterine cancer are age at diagnosis, the [[Stage (cancer)|stage]] of the cancer, the [[Cancer grading|grade]] of the cancer, [[histology]], depth of [[Invasion (cancer)|invasion]] into the myometrium, and the presence of spread to nearby [[lymph node]]s or other regions.<ref>{{cite journal | vauthors = Uharcek P | title = Prognostic factors in endometrial carcinoma | journal = The Journal of Obstetrics and Gynaecology Research | volume = 34 | issue = 5 | pages = 776–783 | date = October 2008 | pmid = 18958927 | doi = 10.1111/j.1447-0756.2008.00796.x | doi-access = free }}</ref> Endometrial cancer typically has a good 5-year-survival when diagnosed early.<ref>{{Cite web|title=Survival Rates for Endometrial Cancer|url=https://www.cancer.org/cancer/endometrial-cancer/detection-diagnosis-staging/survival-rates.html|access-date=2021-09-14|website=www.cancer.org|language=en}}</ref> Generally, the prognosis is poorer for uterine sarcomas as compared to endometrial cancers.<ref>{{Cite web|title=Survival Rates for Uterine Sarcoma|url=https://www.cancer.org/cancer/uterine-sarcoma/detection-diagnosis-staging/survival-rates.html|access-date=2021-09-14|website=www.cancer.org|language=en}}</ref> |
|||
==Epidemiology== |
==Epidemiology== |
||
[[File:Corpus uteri cancer world map - Death - WHO2004.svg|thumb|upright=1.5|[[Age adjustment|Age-standardized]] death from cancer of the uterine body per 100,000 inhabitants in 2004.<ref>{{cite web |url=https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html |title=WHO Disease and injury country estimates |year=2009 |work=World Health Organization |access-date=Nov 11, 2009}}</ref>{{ |
[[File:Corpus uteri cancer world map - Death - WHO2004.svg|thumb|upright=1.5|[[Age adjustment|Age-standardized]] death from cancer of the uterine body per 100,000 inhabitants in 2004.<ref>{{cite web |url=https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html |title=WHO Disease and injury country estimates |year=2009 |work=World Health Organization |access-date=Nov 11, 2009}}</ref>{{Div col|small=yes|colwidth=10em}} |
||
{{legend|#b3b3b3|no data}} |
{{legend|#b3b3b3|no data}} |
||
{{legend|#ffff65|less than 0.5}} |
{{legend|#ffff65|less than 0.5}} |
||
| Line 91: | Line 92: | ||
{{legend|#ff2c00|5–8}} |
{{legend|#ff2c00|5–8}} |
||
{{legend|#cb0000|more than 8}} |
{{legend|#cb0000|more than 8}} |
||
{{ |
{{div col end}}]] |
||
Uterine cancer effects approximately 3.1% of females during their lifetime.<ref name=SEER2019/> Uterine cancer resulted in 45,000 deaths worldwide in 1990, with this number increasing to 58,000 deaths in 2010.<ref name=Loz2012>{{cite journal| |
Uterine cancer effects approximately 3.1% of females during their lifetime.<ref name=SEER2019/> Uterine cancer resulted in 45,000 deaths worldwide in 1990, with this number increasing to 58,000 deaths in 2010.<ref name=Loz2012>{{cite journal | vauthors = Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA | title = Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010 | journal = Lancet | volume = 380 | issue = 9859 | pages = 2095–2128 | date = December 2012 | pmid = 23245604 | pmc = 10790329 | doi = 10.1016/S0140-6736(12)61728-0 | hdl-access = free | s2cid = 1541253 | hdl = 10536/DRO/DU:30050819 }}</ref> North America and Northern Europe have the highest rates of uterine cancer. Asia, Southern Europe, Australia and South America have moderate rates, with the lowest rates in Africa and Eastern Asia.<ref name="Felix_2018">{{cite journal | vauthors = Felix AS, Brinton LA | title = Cancer Progress and Priorities: Uterine Cancer | journal = Cancer Epidemiology, Biomarkers & Prevention | volume = 27 | issue = 9 | pages = 985–994 | date = September 2018 | pmid = 30181320 | pmc = 6504985 | doi = 10.1158/1055-9965.EPI-18-0264 }}</ref> About 81% of women with uterine cancer survive for five years. This rate is higher with more localized cancer at 95% survival rate for five years and lower for a distant spread of the cancer, at a 16.8% survival rate for five years.<ref name=SEER2019/> |
||
===United Kingdom=== |
===United Kingdom=== |
||
Uterine cancer is the fourth most common cancer in females in the UK (around 8,500 women were diagnosed with the disease in 2011), and it is the tenth most common cause of cancer death in females (around 2,000 |
Uterine cancer is the fourth most common cancer in females in the UK (around 8,500 women were diagnosed with the disease in 2011), and it is the tenth most common cause of cancer death in females (around 2,000 women died in 2012).<ref>{{cite web|title=Uterine cancer statistics|url=http://www.cancerresearchuk.org/cancer-info/cancerstats/types/uterus/|website=Cancer Research UK|access-date=28 October 2014}}</ref> |
||
===United States=== |
===United States=== |
||
Uterine cancer has a high prevalence in the United States, with approximately 772,247 |
Uterine cancer has a high prevalence in the United States, with approximately 772,247 women with the disease in 2016.<ref name="SEER" /> Of those uterine cancers, approximately 90% of the cases are endometrial cancers.<ref name="Felix 985–994"/> This is the fourth most commonly diagnosed type of cancer. <ref>{{cite journal | vauthors = Felix AS, Brinton LA | title = Cancer Progress and Priorities: Uterine Cancer | journal = Cancer Epidemiology, Biomarkers & Prevention | volume = 27 | issue = 9 | pages = 985–994 | date = September 2018 | pmid = 30181320 | pmc = 6504985 | doi = 10.1158/1055-9965.EPI-18-0264 }}</ref> |
||
| ⚫ | In the United States, uterine cancer is the most common invasive [[gynecologic cancer]].<ref name="Felix_2018" /> The number of women diagnosed with uterine cancer has been steadily increasing, with 35,040 diagnosed in 1999 and 56,808 diagnosed in 2016. The age-adjusted rate of new cases in 1999 was 23.9 per 100,000 and has increased to 27.3 per 100,000 in 2016.<ref>{{Cite web|url=https://gis.cdc.gov/grasp/USCS/DataViz.html|title=USCS Data Visualizations|website=gis.cdc.gov|language=en|access-date=2019-11-12|archive-date=2019-01-25|archive-url=https://web.archive.org/web/20190125223636/https://gis.cdc.gov/grasp/USCS/DataViz.html|url-status=dead}}</ref> The incidence of uterine cancer increased even more in 2019, with an approximated 61,880 new cases.<ref name="SEER">{{Cite web|url=https://seer.cancer.gov/statfacts/html/corp.html|title=Cancer of the Endometrium - Cancer Stat Facts|website=SEER|language=en|access-date=2019-11-12}}</ref> |
||
| ⚫ | The rates of incidence and death for uterine cancer differ depending on race. The rate of diagnosis is highest for white females, with 28.1 new cases per 100,000 persons. Black females have a similar incidence with 27.4 new cases per 100,000 persons. Other ethnic groups had lower incidences: Hispanic females had 24.1 new cases per 100,000 persons, Asian/Pacific Islander females had 20.8 new cases per 100,000 persons, and American Indian/Alaska Native females had 19.7 new cases per 100,000 persons. For the death rates of uterine cancer, black females had the highest rates, 8.5 deaths per 100,000 persons. The death rates for the other ethnic groups were dramatically lower. White females had 4.4 deaths per 100,000 persons, Hispanic females had 3.9 deaths per 100,000 persons, American Indian/Alaska Native females had 3.5 deaths per 100,000 persons, and Asian/Pacific Islander females had 3.1 deaths per 100,000 persons.<ref name="SEER2019" /> |
||
| ⚫ | In the United States, uterine cancer is the most common invasive gynecologic cancer.<ref name=" |
||
== Research == |
|||
| ⚫ | The rates of incidence and death for uterine cancer differ depending on race. The rate of diagnosis is highest for white females, with 28.1 new cases per 100,000 persons. Black females have a similar incidence with 27.4 new cases per 100,000 persons. Other ethnic groups had lower incidences |
||
As current diagnostic methods are invasive and inaccurate, researchers are looking into new ways to catch womb cancer, especially in its early stages. A study found that using a technique involving [[Infrared|infrared light]] on simple blood test samples detected uterine cancer with high accuracy (87%), and could detect [[Precancerous condition|precancerous growths]] in all cases.<ref>{{Cite journal |date=2020-11-12 |title=Womb cancer could be detected early with an inexpensive new blood test |url=https://evidence.nihr.ac.uk/alert/womb-cancer-could-be-detected-early-with-an-inexpensive-new-blood-test/ |journal=NIHR Evidence |type=Plain English summary |language=en |doi=10.3310/alert_42575|s2cid=241679195 }}</ref><ref>{{cite journal | vauthors = Paraskevaidi M, Morais CL, Ashton KM, Stringfellow HF, McVey RJ, Ryan NA, O'Flynn H, Sivalingam VN, Kitson SJ, MacKintosh ML, Derbyshire AE, Pow C, Raglan O, Lima KM, Kyrgiou M, Martin-Hirsch PL, Martin FL, Crosbie EJ | title = Detecting Endometrial Cancer by Blood Spectroscopy: A Diagnostic Cross-Sectional Study | journal = Cancers | volume = 12 | issue = 5 | pages = 1256 | date = May 2020 | pmid = 32429365 | pmc = 7281323 | doi = 10.3390/cancers12051256 | doi-access = free }}</ref> |
|||
==References== |
== References == |
||
{{Reflist}} |
{{Reflist}} |
||
== External links == |
== External links == |
||
{{Medical resources |
{{Medical resources |
||
| ICD10 = {{ICD10| |
| ICD10 = {{ICD10|C54.1}}{{ICD10|C54.2}} |
||
| ICD9 = |
| ICD9 = |
||
| ICDO = |
| ICDO = |
||
| OMIM = |
| OMIM = |
||
| Line 140: | Line 144: | ||
| incorporated into a formal Bibliography. | |
| incorporated into a formal Bibliography. | |
||
======================= {{No more links}} =============================--> |
======================= {{No more links}} =============================--> |
||
* [ |
* [https://www.cancerresearchuk.org/our-research-by-cancer-type/our-research-into-womb-cancer Clinically reviewed uterine cancer information for patients] |
||
* [http://info.cancerresearchuk.org/cancerstats/types/uterus/ UK uterine cancer statistics] |
* [http://info.cancerresearchuk.org/cancerstats/types/uterus/ UK uterine cancer statistics] |
||
* [https://www.foundationforwomenscancer.org/ Foundation for Women's Caner] |
|||
{{Urogenital neoplasia}} |
{{Urogenital neoplasia}} |
||
Revision as of 19:25, 5 March 2024
| Uterine cancer | |
|---|---|
| Other names | Womb cancer |
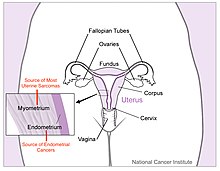 | |
| Diagram of uterus with labeled origins of cancer types. | |
| Specialty | Gynecology, oncology |
| Symptoms | Endometrial cancer: vaginal bleeding, pelvic pain[1] Uterine sarcoma: vaginal bleeding, mass in the vagina[2] |
| Types | Endometrial cancer, uterine sarcoma[3] |
| Risk factors | Endometrial cancer: obesity, metabolic syndrome, type 2 diabetes, tamoxifen use, unopposed estrogens, late menopause, family history of the condition[1] Uterine sarcoma: radiation therapy to the pelvis[2] |
| Treatment | Surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy[1][2] |
| Frequency | 3.8 million (2015)[4] |
| Deaths | 90,000 (2015)[5] |
Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus.[3] Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus.[1][2] Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States.[6] Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis.[1] Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.[2]
Risk factors for endometrial cancer include obesity, metabolic syndrome, type 2 diabetes, taking pills that contain estrogen without progesterone, a history of tamoxifen use, late menopause, and a family history of the condition.[7][1] Risk factors for uterine sarcoma include prior radiation therapy to the pelvis.[2] Diagnosis of endometrial cancer is typically based on an endometrial biopsy.[1] A diagnosis of uterine sarcoma may be suspected based on symptoms, a pelvic exam, and medical imaging.[2]
Endometrial cancer can often be cured while uterine sarcoma typically is harder to treat.[3] Treatment may include a combination of surgery, radiation therapy, chemotherapy, hormone therapy, and targeted therapy.[1][2] Just over 80% of women survive more than 5 years following diagnosis.[8]
In 2015 about 3.8 million women were affected globally and it resulted in 90,000 deaths.[4][5] Endometrial cancer is relatively common while uterine sarcomas are rare.[3] In the United States, uterine cancers represent 3.5% of new cancer cases.[8] They most commonly occur in women between the ages of 45 and 74 with a median age of diagnosis of 63.[8]
Types
The terms uterine cancer and womb cancer may refer to several different types of cancer that occur in the uterus, namely:
- Endometrial carcinomas originate from cells in the glands of the endometrium (uterine lining). These include the common and readily treatable well-differentiated endometrioid adenocarcinoma, as well as the more aggressive uterine papillary serous carcinoma and uterine clear-cell carcinoma.[9]
- Malignant mixed Müllerian tumors (also known as uterine carcinosarcomas) are rare endometrial tumors which show both glandular (carcinomatous) and stromal (sarcomatous) differentiation.[9]
- Leiomyosarcomas originate from the muscular layer of the uterus (or myometrium). Of note, leiomyosarcomas are distinct from uterine leiomyomas, which are benign tumors of the uterus.[10]
- Endometrial stromal sarcomas originate from the connective tissues of the endometrium, and are far less common than endometrial carcinomas.[10]
Signs and symptoms
Both types of uterine cancer can present with abnormal vaginal bleeding and discharge.[11][12] Abnormalities can include change in duration or amount of menstrual bleeding as well as new bleeding between menses or after menopause. Sensations of new or increasing pelvic pressure or pain can also indicate tumor growth in the uterus.[12] Any of these findings warrant further workup by a doctor.
Causes and risk factors
It is not known with certainty what the causes for uterine cancer may be, though hormone imbalance is cited as a risk factor. Estrogen receptors, known to be present on the surfaces of cells of this type of cancer, are thought to interact with the hormone causing increased cell growth, which can then result in cancer. The exact mechanism of how this occurs is not understood.[13]
Risk factors for endometrial cancer include obesity, metabolic syndrome, type 2 diabetes, taking pills that contain estrogen without progesterone, a history of tamoxifen use, late menopause, and certain hereditary conditions (Lynch syndrome, Cowden syndrome).[7][1][11] Risk factors for uterine sarcoma include prior radiation therapy to the pelvis, a history of tamoxifen use, a history of childhood retinoblastoma, and hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome.[2][12]
Diagnosis
To evaluate for uterine cancer, a clinician might perform a pelvic exam to visually inspect internal pelvic organs and to feel the size and position of the uterus and ovaries. A “pap smear” may also be done to brush the sides of the cervix to collect cells for testing and to look at under a microscope. A dilatation and curettage is often done to collect a sample of uterine lining tissue. An ultrasound is also often performed to look for tumors.[14]
Screening and Prevention
Screening for uterine cancers is not recommended except for in women with certain hereditary conditions that increase their risk (Lynch, Cowden, HLRCC).[11][12]
In general, combined oral contraceptive pills and progestin-only pills are protective against uterine cancers. Weight loss and/or bariatric surgery reduces the risk for patients with obesity.[11]
Treatment
Treatment of uterine cancer may differ depending on the type of cancer and staging of the tumor.[15] In early stages, minimal invasive surgery is preferred. [16]
For endometrial cancer, five main types of treatments are used, including surgery, radiation therapy, chemotherapy, hormone therapy, and targeted therapy. The most common treatment modality for endometrial cancer is surgery, whereby the uterus is removed via a total hysterectomy.[15] Hysterectomies may also be accompanied by removal of ovaries and fallopian tubes, called a salpingo-oophorectomy. Additionally, hormone therapy which seeks to block the growth of cancer cells may also be used in the treatment of endometrial cancer. Targeted therapy may include monoclonal antibodies, mTOR inhibitors, and signal transduction inhibitors which all act to target cancer cells specifically.[15]
As of 2021, treatment options for uterine sarcoma include surgery, radiation therapy, chemotherapy, and hormone therapy.[15]
Prognosis
Prognosis varies for the different types of endometrial cancer. Factors that influence prognosis across types of uterine cancer are age at diagnosis, the stage of the cancer, the grade of the cancer, histology, depth of invasion into the myometrium, and the presence of spread to nearby lymph nodes or other regions.[17] Endometrial cancer typically has a good 5-year-survival when diagnosed early.[18] Generally, the prognosis is poorer for uterine sarcomas as compared to endometrial cancers.[19]
Epidemiology

Uterine cancer effects approximately 3.1% of females during their lifetime.[8] Uterine cancer resulted in 45,000 deaths worldwide in 1990, with this number increasing to 58,000 deaths in 2010.[21] North America and Northern Europe have the highest rates of uterine cancer. Asia, Southern Europe, Australia and South America have moderate rates, with the lowest rates in Africa and Eastern Asia.[22] About 81% of women with uterine cancer survive for five years. This rate is higher with more localized cancer at 95% survival rate for five years and lower for a distant spread of the cancer, at a 16.8% survival rate for five years.[8]
Vereinigtes Königreich
Uterine cancer is the fourth most common cancer in females in the UK (around 8,500 women were diagnosed with the disease in 2011), and it is the tenth most common cause of cancer death in females (around 2,000 women died in 2012).[23]
Vereinigte Staaten
Uterine cancer has a high prevalence in the United States, with approximately 772,247 women with the disease in 2016.[24] Of those uterine cancers, approximately 90% of the cases are endometrial cancers.[6] This is the fourth most commonly diagnosed type of cancer. [25]
In the United States, uterine cancer is the most common invasive gynecologic cancer.[22] The number of women diagnosed with uterine cancer has been steadily increasing, with 35,040 diagnosed in 1999 and 56,808 diagnosed in 2016. The age-adjusted rate of new cases in 1999 was 23.9 per 100,000 and has increased to 27.3 per 100,000 in 2016.[26] The incidence of uterine cancer increased even more in 2019, with an approximated 61,880 new cases.[24]
The rates of incidence and death for uterine cancer differ depending on race. The rate of diagnosis is highest for white females, with 28.1 new cases per 100,000 persons. Black females have a similar incidence with 27.4 new cases per 100,000 persons. Other ethnic groups had lower incidences: Hispanic females had 24.1 new cases per 100,000 persons, Asian/Pacific Islander females had 20.8 new cases per 100,000 persons, and American Indian/Alaska Native females had 19.7 new cases per 100,000 persons. For the death rates of uterine cancer, black females had the highest rates, 8.5 deaths per 100,000 persons. The death rates for the other ethnic groups were dramatically lower. White females had 4.4 deaths per 100,000 persons, Hispanic females had 3.9 deaths per 100,000 persons, American Indian/Alaska Native females had 3.5 deaths per 100,000 persons, and Asian/Pacific Islander females had 3.1 deaths per 100,000 persons.[8]
Forschung
As current diagnostic methods are invasive and inaccurate, researchers are looking into new ways to catch womb cancer, especially in its early stages. A study found that using a technique involving infrared light on simple blood test samples detected uterine cancer with high accuracy (87%), and could detect precancerous growths in all cases.[27][28]
References
- ^ a b c d e f g h i "Endometrial Cancer Treatment". National Cancer Institute. 26 April 2018. Retrieved 3 February 2019.
- ^ a b c d e f g h i "Uterine Sarcoma Treatment". National Cancer Institute. 3 October 2018. Retrieved 3 February 2019.
- ^ a b c d "Uterine Cancer". National Cancer Institute. 1 January 1980. Retrieved 3 February 2019.
- ^ a b "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. October 2016. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ a b "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. October 2016. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ a b Felix AS, Brinton LA (September 2018). "Cancer Progress and Priorities: Uterine Cancer". Cancer Epidemiology, Biomarkers & Prevention. 27 (9): 985–994. doi:10.1158/1055-9965.EPI-18-0264. PMC 6504985. PMID 30181320.
- ^ a b "Endometrial Cancer Risk Factors". www.cancer.org. Retrieved 2021-09-13.
- ^ a b c d e f "Uterine Cancer - Cancer Stat Facts". SEER. Retrieved 3 February 2019.
- ^ a b "What Is Endometrial Cancer?". www.cancer.org. Retrieved 2021-09-14.
- ^ a b "What Is Uterine Sarcoma?". www.cancer.org. Retrieved 2021-09-14.
- ^ a b c d "Endometrial carcinoma: Clinical features, diagnosis, prognosis, and screening". www.uptodate.com. Retrieved 2021-09-18.
- ^ a b c d "Uterine sarcoma: Classification, epidemiology, clinical manifestations, and diagnosis". www.uptodate.com. Retrieved 2021-09-18.
- ^ Causes, Risk Factors, and Prevention TOPICS - Do we know what causes endometrial cancer? - cancer.org - American Cancer Society - Retrieved 5 January 2015.
- ^ "Uterine Cancer - Diagnosis". Cancer.Net. 2012-06-25. Retrieved 2021-09-14.
- ^ a b c d "Uterine Cancer—Patient Version - National Cancer Institute". www.cancer.gov. Retrieved 2021-09-13.
- ^ Filippova OT, Leitao MM (July 2020). "The current clinical approach to newly diagnosed uterine cancer". Expert Review of Anticancer Therapy. 20 (7): 581–590. doi:10.1080/14737140.2020.1782750. PMC 7416456. PMID 32531179.
- ^ Uharcek P (October 2008). "Prognostic factors in endometrial carcinoma". The Journal of Obstetrics and Gynaecology Research. 34 (5): 776–783. doi:10.1111/j.1447-0756.2008.00796.x. PMID 18958927.
- ^ "Survival Rates for Endometrial Cancer". www.cancer.org. Retrieved 2021-09-14.
- ^ "Survival Rates for Uterine Sarcoma". www.cancer.org. Retrieved 2021-09-14.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov 11, 2009.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ a b Felix AS, Brinton LA (September 2018). "Cancer Progress and Priorities: Uterine Cancer". Cancer Epidemiology, Biomarkers & Prevention. 27 (9): 985–994. doi:10.1158/1055-9965.EPI-18-0264. PMC 6504985. PMID 30181320.
- ^ "Uterine cancer statistics". Cancer Research UK. Retrieved 28 October 2014.
- ^ a b "Cancer of the Endometrium - Cancer Stat Facts". SEER. Retrieved 2019-11-12.
- ^ Felix AS, Brinton LA (September 2018). "Cancer Progress and Priorities: Uterine Cancer". Cancer Epidemiology, Biomarkers & Prevention. 27 (9): 985–994. doi:10.1158/1055-9965.EPI-18-0264. PMC 6504985. PMID 30181320.
- ^ "USCS Data Visualizations". gis.cdc.gov. Archived from the original on 2019-01-25. Retrieved 2019-11-12.
- ^ "Womb cancer could be detected early with an inexpensive new blood test". NIHR Evidence (Plain English summary). 2020-11-12. doi:10.3310/alert_42575. S2CID 241679195.
- ^ Paraskevaidi M, Morais CL, Ashton KM, Stringfellow HF, McVey RJ, Ryan NA, et al. (May 2020). "Detecting Endometrial Cancer by Blood Spectroscopy: A Diagnostic Cross-Sectional Study". Cancers. 12 (5): 1256. doi:10.3390/cancers12051256. PMC 7281323. PMID 32429365.
