Flap (surgery): Difference between revisions
FinnSoThin (talk | contribs) No edit summary Tags: Mobile edit Mobile app edit iOS app edit |
BrayLockBoy (talk | contribs) No edit summary |
||
| (30 intermediate revisions by 14 users not shown) | |||
| Line 3: | Line 3: | ||
Name = Flap surgery | |
Name = Flap surgery | |
||
Image = Erichsen Flap.jpg| |
Image = Erichsen Flap.jpg| |
||
Caption = |
Caption = Engraving by [[John Eric Erichsen]] depicting flap surgery used to cover an [[amputation]] stump| |
||
ICD10 = | |
ICD10 = | |
||
ICD9 = 86.7| |
ICD9 = 86.7| |
||
| Line 10: | Line 10: | ||
}} |
}} |
||
'''Flap surgery''' is a technique in [[plastic surgery|plastic]] and [[reconstructive surgery]] where |
'''Flap surgery''' is a technique in [[plastic surgery|plastic]] and [[reconstructive surgery]] where [[Tissue (biology)|tissue]] with an intact [[blood supply]] is lifted from a donor site and moved to a recipient site. Flaps are distinct from [[Graft (surgery)|grafts]], which do not have an intact blood supply and relies on the growth of new blood vessels. Flaps are done to fill a defect such as a wound resulting from injury or surgery when the remaining tissue is unable to support a graft, or to rebuild more complex anatomic structures like breasts or jaws.<ref name="EssentialsForStudents" /><ref name="Chung_2020" /> |
||
{{TOC limit|3}} |
|||
== Uses == |
== Uses == |
||
Flap surgery is a technique essential to [[Plastic surgery|plastic]] and [[ |
Flap surgery is a technique essential to [[Plastic surgery|plastic]] and [[reconstructive surgery]]. A flap is defined as tissue that can be moved to another site and has its own [[Circulatory system|blood supply]]. This is in comparison to a [[Skin grafting|skin graft]] which does not have its own blood supply and relies on [[Angiogenesis|vascularization]] from the recipient site.<ref name="Chung_2020" /> Flaps have many uses in [[wound healing]] and are used when wounds are large, complex, or need tissue and bulk for successful closure.<ref name="Chung_2020" /> |
||
Common uses: |
|||
* Abdominal wall reconstruction |
|||
* [[Breast reconstruction]] |
|||
* [[Hand surgery|Hand reconstruction]] |
|||
* [[Mandible|Mandible reconstruction]] |
|||
* [[Rhinoplasty]] |
|||
* [[Scar]] revision |
|||
* [[Skin cancer]] |
|||
==Anatomy== |
==Anatomy== |
||
Flaps can contain many different combination of layers of tissue, from skin to bone (see {{Section link|2=Classification|nopage=y}}). The main goal of a flap is to maintain blood flow to tissue to maintain survival, and understanding the anatomy in flap design is key to a successful flap surgery.<ref name="Chung_2020" /> |
|||
=== Anatomy of a flap === |
|||
"Plastic surgery is a constant battle between blood supply and beauty." - [[Harold Gillies|Sir Harold Gillies]]<ref>{{Cite book |last=Gillies |first=H.D. |title=The Principles and Art of Plastic Surgery |last2=Millard |first2=D. Ralph |publisher=Little, Brown and Company |year=1957 |volume=2}}</ref> |
|||
[[File:Gray942.png|thumb|The distribution of the blood vessels in the skin of the [[sole of the foot]]. The [[dermis]] is referred to as ''corium''.]] |
|||
=== Skin anatomy === |
=== Skin anatomy === |
||
{{See also|Human skin#Skin layers|l1=Human skin layers}} |
|||
{{See also|Human skin#Skin layers|l1=Human skin layers}}Flaps may include skin in their construction. Skin is important for many reasons, but namely its role in [[thermoregulation]], [[Immune system|immune function]], and blood supply aid in flap survival.<ref name=":4" /> The skin can be divided into three main layers including the [[epidermis]], the [[dermis]], and the [[subcutaneous tissue]]. Blood is supplied to the skin mainly by two networks of blood vessels. The deep network lies between the dermis and the [[subcutaneous tissue]], while the shallow network lies within the papillary layer of the dermis.<ref name="Guyuron8.3"/> The epidermis is supplied by diffusion from this shallow network and both networks are supplied by [[collateral circulation|collaterals]], and by perforating arteries that bring blood from deeper layers either between muscles (septocutaneous perforators) or through muscles (musculocutaneous perforators).<ref name=":4" /> |
|||
Flaps may include skin in their construction. Skin is important for many reasons, but namely its role in [[thermoregulation]], [[immune function]], and blood supply aid in flap survival.<ref name="Chung_2020"/> The skin can be divided into three main layers: the [[epidermis]], [[dermis]], and [[subcutaneous tissue]]. Blood is mainly supplied to the skin by two networks of blood vessels. The deep network lies between the dermis and the subcutaneous tissue, while the shallow network lies within the papillary layer of the dermis.<ref name="pmid11735064"/> The epidermis is supplied by diffusion from this shallow network and both networks are supplied by [[collateral circulation|collaterals]], and by perforating arteries that bring blood from deeper layers either between muscles (septocutaneous perforators) or through muscles (musculocutaneous perforators).<ref name="Chung_2020"/> |
|||
This robust and redundant blood supply is important in flap surgery |
This robust and redundant blood supply is important in flap surgery,<ref name="Chung_2020"/> because flaps are cut off from other blood vessels when it is raised and removed from its surrounding native tissue.<ref name="Chung_2020"/> The remaining blood supply must then keep the tissue alive until additional blood supply can be formed through [[angiogenesis]].<ref name="Guyuron8" /> |
||
=== Angiosome === |
=== Angiosome === |
||
The [[angiosome]] is a concept first coined by Ian Taylor in 1987.<ref |
The [[angiosome]] is a concept first coined by Ian Taylor in 1987.<ref name="pmid3567445"/> It is a three-dimensional region of tissue that is supplied by a single artery and can include skin, soft tissue, and bone.<ref name="pmid3567445"/><ref name="pmid10845282"/> Adjacent angiosomes are connected by narrower choke vessels, and multiple angiosomes can be supplied by a single artery. Knowledge of these supply arteries and their associated angiosomes is useful in planning the location, size, and shape of a flap.<ref name="Guyuron8" /> |
||
{{Clear}} |
{{Clear}} |
||
| Line 47: | Line 36: | ||
{{Further|List of plastic surgery flaps}} |
{{Further|List of plastic surgery flaps}} |
||
Flaps can be fundamentally classified by their mechanism of movement, the types of tissues present, or by their blood supply.<ref name=" |
Flaps can be fundamentally classified by their mechanism of movement, the types of tissues present, or by their blood supply.<ref name="Chung_2020"/> The surgeon generally chooses the least complex type that will achieve the desired effect via a concept known as the [[reconstructive ladder]].<ref name="pmid16816714"/><ref name="pmid16565127"/> |
||
===Mechanism of movement=== |
===Mechanism of movement=== |
||
| Line 64: | Line 53: | ||
}} |
}} |
||
* Local flaps are created by freeing a layer of tissue and then stretching the freed layer to fill a defect. This is the least complex type of flap and includes advancement flaps, rotation flaps, and transposition flaps, in order from least to most complex. With an advancement flap, incisions are extended out parallel from the wound, creating a rectangle with one edge remaining intact. This rectangle is freed from the deeper tissues and then stretched (or advanced) forward to cover the wound. The flap is disconnected from the body except for the uncut edge which contains the blood supply which feeds in horizontally. A rotation flap is similar except instead of being stretched in a straight line, the flap is stretched in an arc. The more complex transposition flap involves rotating an adjacent piece of tissue, resulting in the creation of a new defect that must then be closed.<ref name="Guyuron8" /> |
|||
==== Local flaps ==== |
|||
* Regional or interpolation flaps are not immediately adjacent to the defect. Instead, the freed tissue "island" is moved over or underneath normal tissue to reach the defect to be filled, with the blood supply still connected to the donor site via a pedicle.<ref name="pmid15620622"/> The pedicle can be removed after a new blood supply has formed. Examples: [[pectoralis major]] myocutaneous flap and deltopectoral flap for head and neck defects, and [[Latissimus dorsi muscle|latissimus dorsi]] flap and [[TRAM flap|traverse rectus abdominal muscle (TRAM) flap]] for breast reconstruction.<ref name="Guyuron8" /> |
|||
* Local flaps are created by freeing a layer of tissue and then stretching the freed layer to fill a defect. This is the least complex type of flap and includes advancement flaps, rotation flaps, and transposition flaps, in order from least to most complex. With an advancement flap, incisions are extended out parallel from the wound, creating a rectangle with one edge remaining intact. This rectangle is freed from the deeper tissues and then stretched (or ''advanced'') forward to cover the wound. The flap is disconnected from the body except for the uncut edge which contains the blood supply which feeds in horizontally. A rotation flap is similar except instead of being stretched in a straight line, the flap is stretched in an arc. The more complex transposition flap involves rotating an adjacent piece of tissue, resulting in the creation of a new defect that must then be closed.<ref name="Guyuron8" /> |
|||
* Distant flaps are used when the donor site is far from the defect. These are the most complex class of flap. Direct or tubed flaps involve having the flap connected to both the donor and recipient sites simultaneously, forming a bridge. This allows blood to be supplied by the donor site while a new blood supply from the recipient site is formed. Once this happens, the bridge can be disconnected from the donor site if necessary, completing the transfer.<ref name="pmid15814122"/> A [[free flap]] has the blood supply cut and then reattached [[microsurgery|microsurgically]] to a new blood supply at the recipient site.<ref name="Guyuron9" /><ref name="Wolf_2011"/> |
|||
====Regional flaps==== |
|||
* Regional or interpolation flaps are not immediately adjacent to the defect. Instead, the freed tissue "island" is moved over or underneath normal tissue to reach the defect to be filled, with the blood supply still connected to the donor site via a pedicle.<ref name="Guyuron8.38" /> This pedicle can be removed later on after new blood supply has formed. Examples: pectoralis major myocutaneous (PMMC) flap and deltopectoral (DP) flap for head and neck defects, and latissimus dorsi (LD) flap and traverse rectus abdominal muscle (TRAM) flap for breast reconstruction.<ref name="Guyuron8" /> |
|||
====Distant flaps==== |
|||
* Distant flaps are used when the donor site is far from the defect. These are the most complex class of flap. Direct or tubed flaps involve having the flap connected to both the donor and recipient sites simultaneously, forming a bridge. This allows blood to be supplied by the donor site while a new blood supply from the recipient site is formed. Once this happens, the "bridge" can be disconnected from the donor site if necessary, completing the transfer.<ref name="Guyuron8.41" /> A [[free flap]] has the blood supply cut and then reattached [[microsurgery|microsurgically]] to a new blood supply at the recipient site.<ref name="Guyuron9" /><ref name=":2" /> |
|||
===Tissue type=== |
===Tissue type=== |
||
Flaps can be classified by the content of the tissue within them. |
Flaps can be classified by the content of the tissue within them. |
||
* Cutaneous flaps contain the full thickness of the skin, fat, and superficial fascia and are used to fill small defects. These are typically supplied by a random blood supply. Examples include [[Z-plasty]], [[DIEP flap|deep inferior epigastric perforator (DIEP) flaps]], and V-Y advancement flaps.<ref name="Chung_2020"/> |
|||
==== Cutaneous ==== |
|||
* Fasciocutaneous flaps contain subcutaneous tissue and deep fascia, resulting in a more robust blood supply and ability to fill a larger defect. The Cormack and Lamberty classification is used for the vascular supply of faciocutaneous flaps.<ref name="pmid6692066"/> Examples: temporoparietal and anterolateral thigh fascocutaneous flap, lateral fasciocutaneous flap, posterior fasciocutaneous flap.<ref name="Chung_2020"/> |
|||
* Contain the full thickness of the skin, fat, and superficial fascia and are used to fill small defects. These are typically supplied by a random blood supply. Examples: [[Z-plasty]], [[DIEP flap|deep inferior epigastric perforator (DIEP) flap]], V-Y advancement flap.<ref name=":4" /> |
|||
==== Fasciocutaneous ==== |
|||
* Contain subcutaneous tissue and deep fascia, resulting in a more robust blood supply and ability to fill a larger defect. Cormack and Lamberty classification is used for vascular supply of faciocutaneous flaps.<ref>{{Cite journal |last=Cormack |first=G. C. |last2=Lamberty |first2=B. G. |date=January 1984 |title=A classification of fascio-cutaneous flaps according to their patterns of vascularisation |url=https://pubmed.ncbi.nlm.nih.gov/6692066 |journal=British Journal of Plastic Surgery |volume=37 |issue=1 |pages=80–87 |doi=10.1016/0007-1226(84)90049-3 |issn=0007-1226 |pmid=6692066}}</ref> Examples: temporoparietal and anterolateral thigh fascocutaneous flap, lateral fasciocutaneous flap, posterior fasciocutaneous flap.<ref name=":4" /> |
|||
[[File:Diagram showing breast reconstruction using the latissimus dorsi muscle and an implant CRUK 405.svg|thumb|368x368px|Breast reconstruction using the latissimus dorsi muscle and an implant. This is an example of a pedicled musculocutaneous flap.]] |
[[File:Diagram showing breast reconstruction using the latissimus dorsi muscle and an implant CRUK 405.svg|thumb|368x368px|Breast reconstruction using the latissimus dorsi muscle and an implant. This is an example of a pedicled musculocutaneous flap.]] |
||
* Musculocutaneous and muscle flaps contain a layer of [[Skeletal muscle|muscle]] to provide bulk that can fill a deeper defect. If skin cover is needed, a [[skin graft]] can be placed over top of it. Examples: [[gastrocnemius]] flap, latissimus dorsi flap, TRAM flap, and [[Free flap breast reconstruction#TMG flap/TUG flap — Transverse Myocutaneous/Upper Gracilis flap|transverse upper gracillis flap]].<ref name="Chung_2020"/> |
|||
==== Musculocutaneous and Muscle flaps ==== |
|||
* Contain a layer of muscle to provide bulk that can fill a deeper defect. If skin cover is needed, a [[skin graft]] can be placed over top of it. Examples: [[gastrocnemius]] flap, [[Latissimus dorsi muscle|latissimus dorsi]] flap, [[TRAM flap|transverse rectus abdominis myocutaneous (TRAM) flap]], [[Free flap breast reconstruction#TMG flap/TUG flap %E2%80%94 Transverse Myocutaneous/Upper Gracilis flap|transverse upper gracillis (TUG) flap]].<ref name=":4" /> |
|||
==== Bone ==== |
|||
* Contain bone and are used when structural support is needed such as in jaw reconstruction. Example: fibula flap.<ref name=":4" /><ref name="Guyuron8" /><ref name="Guyuron8.2" /> |
|||
* Bone flaps contain bone and are used when structural support is needed such as in jaw reconstruction. Example: fibula flap.<ref name="Chung_2020"/><ref name="Guyuron8" /><ref name="Guyuron8.2" /> |
|||
==== Omental and Intestinal ==== |
|||
*Omental flaps can be used in chest wall defects and intestinal flaps can be used to reconstruct tubular structures like the esophagus.<ref name=" |
*[[Lesser sac|Omental]] flaps can be used in chest wall defects, and [[intestinal]] flaps can be used to reconstruct tubular structures like the esophagus.<ref name="Chung_2020"/> |
||
===Vascular supply=== |
===Vascular supply=== |
||
Classification based on blood supply to the flap: |
Classification based on blood supply to the flap: |
||
* Axial flaps are supplied by a named [[artery]] and [[vein]]. This allows for a larger area to be freed from surrounding and underlying tissue, leaving only a small pedicle containing the vessels.<ref name="Chung_2020"/> Reverse-flow flaps are a type of axial flap in which the supply artery is cut on one end and blood is supplied by backwards flow from the other direction. Random flaps are simpler and have no named blood supply; they are supplied by the subdermal plexus.<ref name="pmid11735064" /><ref name="Guyuron8" /> |
|||
* Pedicled flaps remain attached to the donor site via a pedicle that contains the blood supply, in contrast to a free flap, where the vessels are cut and [[Anastomosis|anastomosed]] to another blood supply.<ref name="EssentialsForStudents" /><ref name="Chung_2020"/> |
|||
==== Axial vs random ==== |
|||
* Axial flaps are supplied by a named artery and vein. This allows for a larger area to be freed from surrounding and underlying tissue, leaving only a small pedicle containing the vessels.<ref name=":4" /> Reverse-flow flaps are a type of axial flap in which the supply artery is cut on one end and blood is supplied by backwards flow from the other direction. Random flaps are simpler and have no named blood supply. Rather, they are supplied by generic vascular networks.<ref name="Guyuron8.3" /><ref name="Guyuron8" /> |
|||
==== Pedicled vs free ==== |
|||
* Pedicled flaps remain attached to the donor site via a pedicle that contains the blood supply, in contrast to a free flap which the vessels are cut and [[Anastomosis|anastomosed]] to another blood supply.<ref name="EssentialsForStudents" /><ref name=":4" /> |
|||
== Contraindications == |
== Contraindications == |
||
Anyone who is unstable for surgery should not undergo flap surgery |
Anyone who is unstable for surgery should not undergo flap surgery. As with most surgeries, people who are sicker may have more difficulties with [[wound healing]], which include individuals with [[Comorbidity|comorbidities]] such as [[diabetes]], [[Tobacco smoking|smoking]], [[immunosuppression]], and [[vascular disease]].<ref name="Carrau_2008"/><ref name="pmid23190838"/> |
||
== Risks or complications== |
== Risks or complications== |
||
The risks of flap surgery include infection |
The risks of flap surgery include infection, [[Wound dehiscence|wound breakdown]], [[Seroma|fluid accumulation]], [[bleeding]], damage to nearby structures, and [[scar]]ring.<ref name="pmid15814122"/> The most notable risk in this procedure is flap death, where the flap loses blood supply. The loss of blood can be due to many reasons, but is commonly due to tension on the vascular supply and insufficient blood flow to the end segments of the flap.<ref name="pmid15814122"/> This can sometimes be fixed with another surgery or using additional methods of healing in the reconstructive ladder.<ref name="pmid7661898"/> |
||
== Recovery == |
== Recovery == |
||
{{See also|Wound healing}} |
{{See also|Wound healing}} |
||
As with healing of any wound, healing of a flap maintains the same process |
As with healing of any wound, healing of a flap maintains the same process of wound healing. There are four stages to wound healing: [[hemostasis]], [[inflammation]], [[Cell proliferation|proliferation]], and [[Cellular differentiation|remodeling]], all of which can take up to a year to complete.<ref name="pmid27556770"/><ref name="Chung_2020"/> |
||
Following flap surgery, the biggest risk in recovery is flap death. Flap failure is an uncommon occurrence but does happen. The reported flap failure rate in free flaps is less than 5%.<ref name=" |
Following flap surgery, the biggest risk in recovery is flap death. Flap failure is an uncommon occurrence but does happen. The reported flap failure rate in free flaps is less than 5%.<ref name="pmid8942909"/> The most commonly cause is by [[Venous stasis|venous insufficiency]] consisting of 54% of all causes.<ref name="pmid8942909"/> Venous insufficiency is commonly caused by a [[Venous thrombosis|venous thrombus]] within the first 2 days following surgery.<ref name="pmid8942909"/><ref name="pmid27556770"/> After the immediate postoperative risk, the flap will continue to heal adhering to the stages of normal wound healing and will take over 3 months for an incision to be at 80% tensile strength compared to normal tissue.<ref name="pmid27556770"/> |
||
[[File:Walter Yeo skin graft.jpg|thumb|238x238px|[[Walter Yeo]], the first person to receive plastic surgery, before (left) and after (right) skin flap surgery performed by [[Harold Gillies]] in 1917. The surgery was some of the first to use a skin flap from an unaffected area of the body and paved the way for a sudden rash of improvements in this field.]] |
|||
== History == |
== History == |
||
Skin flaps are an essential part of a surgeon's toolbox in plastic surgery. It is part of the reconstructive ladder.<ref name="pmid7661898"/> The first known reports of surgical flaps originated in 600 BC in India by [[Sushruta Samhita|Sushruta]] where the tilemakers' caste would reconstruct noses using regional flaps due to the practice of nose amputations as a form of legal punishment.<ref name="pmid20431512"/><ref name="pmid7661898"/> The next description of flap surgery comes from Celsus, an ancient Roman who described the advancement of skin flaps from 25 BC to 50 AD.<ref name="pmid20431512"/><ref name="pmid7661898"/> In the 15th century, [[Gaspare Tagliacozzi]], an Italian surgeon, helped develop the "Italian method" for nasal reconstruction, a delayed pedicle skin graft, where the skin from the arm would be attached to the nose for many months to create the reconstruction, first printed in the 1597 book ''De Curtorum Chirurgia per Insitionem''.<ref name="pmid24610608"/> The Italian method was rediscovered in 1800 by German surgeon [[Karl Ferdinand von Gräfe|Carl Ferdinand von Graefe]].<ref name="Erovic_2015"/> Major advancements in modern plastic surgery are mostly attributed to [[Harold Gillies]], who pioneered facial reconstruction during World War I using pedicled tube flaps on patients like [[Walter Yeo]], and the development of the [[walking-stalk skin flap]] by Gilles' cousin [[Archibald McIndoe]] in 1930.<ref name="pmid20431512"/><ref name="Gillies_2019"/> |
|||
Skin flaps are an essential part of a surgeon’s toolbox in [[Plastic surgery|Plastic Surgery]]. It is part of the [[reconstructive ladder]], a stepwise approach to wound closure.<ref name=":1">{{Cite journal |last=Gottlieb |first=Lawrene J. |last2=Krieger |first2=Lloyd M. |date=June 1994 |title=From the Reconstructive Ladder to the Reconstructive Elevator: |url=http://journals.lww.com/00006534-199406000-00027 |journal=Plastic and Reconstructive Surgery |language=en |volume=93 |issue=7 |pages=1503 |doi=10.1097/00006534-199406000-00027 |issn=0032-1052}}</ref> |
|||
Advancements continued in flap surgery. With the introduction of the [[operating microscope]], microvascular surgery advancements allowed for the anastomosis of blood vessels.<ref name="Wolf_2011"/> This led to the ability of free tissue transfers, and in 1958 Bernard Seidenberg transferred a part of the [[jejunum]] to the [[esophagus]] to remove a [[cancer]].<ref name="Wolf_2011"/><ref name="pmid13627972"/> Modern advancements in flap surgeries have continued since this time and are now commonly used in many procedures.<ref name="Wolf_2011"/> |
|||
The first known reports of surgical flaps originated in 600 BCE in India by [[Sushruta Samhita|Sushruta]] where the Tilemakers caste would reconstruct noses using regional flaps due to the practice of nose amputations as a form of legal punishment.<ref name=":0">{{Cite journal |last=Chambers |first=James Alan |last2=Ray |first2=Peter Damian |date=November 2009 |title=Achieving Growth and Excellence in Medicine: The Case History of Armed Conflict and Modern Reconstructive Surgery |url=https://journals.lww.com/00000637-200911000-00002 |journal=Annals of Plastic Surgery |language=en |volume=63 |issue=5 |pages=473–478 |doi=10.1097/SAP.0b013e3181bc327a |issn=0148-7043}}</ref><ref name=":1" /> The next description of flap surgery comes from Celsus an ancient Roman who described advancement skin flaps from 25 BC to 50 AD.<ref name=":0" /><ref name=":1" /> In the 15th century, [[Gaspare Tagliacozzi]] an Italian surgeon helped develop the “Italian Method” for nasal reconstruction, a delayed pedicle skin graft, where the skin from the arm would be attached to the nose for many months to create the reconstruction, first printed in the 1597 book ''De Curtorum Chirurgia per Insitionem''.<ref>{{Cite journal |last=Tomba |first=P. |last2=Viganò |first2=A. |last3=Ruggieri |first3=P. |last4=Gasbarrini |first4=A. |date=2014 |title=Gaspare Tagliacozzi, pioneer of plastic surgery and the spread of his technique throughout Europe in "De Curtorum Chirurgia per Insitionem" |url=https://pubmed.ncbi.nlm.nih.gov/24610608 |journal=European Review for Medical and Pharmacological Sciences |volume=18 |issue=4 |pages=445–450 |issn=2284-0729 |pmid=24610608}}</ref> The Italian method was rediscovered in 1800 by German surgeon [[Karl Ferdinand von Gräfe|Carl Ferdinand von Graefe]].<ref>{{Cite book |last=M. |first=Erovic, Boban |url=http://worldcat.org/oclc/974391518 |title=Manual of Head and Neck Reconstruction Using Regional and Free Flaps |date=2015 |publisher=Springer Vienna |isbn=978-3-7091-1172-7 |oclc=974391518}}</ref> Major advancements in modern Plastic Surgery are mostly attributed to [[Harold Gillies|Harold Gilles]] who pioneered facial reconstruction during World War I using pedicled tube flaps on patients such as [[Walter Yeo]] and the development of the [[walking-stalk skin flap]] by Gilles' cousin [[Archibald McIndoe]] in 1930.<ref name=":0" /><ref>{{Cite book |last=Gillies |first=H. D. |url=http://worldcat.org/oclc/1152260318 |title=Plastic Surgery of the Face Based on Selected Cases of War Injuries of the Face, Including Burns; With Original Illustrations |isbn=978-0-259-73591-5 |oclc=1152260318}}</ref> |
|||
Advancements continued in flap surgery. With the introduction of the [[Operating microscope|Operating Microscope]] Microvascular surgery advancements allowed for the [[anastomosis]] of blood vessels.<ref name=":2">{{Cite book |last=Wolff |first=Klaus-Dietrich |url=https://www.worldcat.org/oclc/733542624 |title=Raising of microvascular flaps: a systematic approach |date= |publisher=Springer |others=F. Hölzle |year=2011 |isbn=978-3-642-13831-7 |edition=2nd |location=Berlin |oclc=733542624}}</ref> This led to the ability of free tissue transfers and in 1958 Bernard Seidenberg transferred a part of the [[jejunum]] to the [[esophagus]] to remove a [[cancer]] of the esophagus.<ref name=":2" /><ref>{{Cite journal |last=Seidenberg |first=B. |last2=Rosenak |first2=S. S. |last3=Hurwitt |first3=E. S. |last4=Som |first4=M. L. |date=February 1959 |title=Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment |url=https://pubmed.ncbi.nlm.nih.gov/13627972 |journal=Annals of Surgery |volume=149 |issue=2 |pages=162–171 |doi=10.1097/00000658-195902000-00002 |issn=0003-4932 |pmc=1450976 |pmid=13627972}}</ref> Modern advancements in flap surgeries have continued since this time and are now commonly used in many procedures.<ref name=":2" /> |
|||
==See also== |
==See also== |
||
* [[Breast reconstruction]] |
* [[Breast reconstruction]] |
||
* [[DIEP flap]] |
* [[DIEP flap]] |
||
* [[Hand surgery |
* [[Hand surgery]] |
||
* [[List of plastic surgery flaps]] |
* [[List of plastic surgery flaps]] |
||
* [[Plastic surgery]] |
|||
* [[Perforator flaps]] |
* [[Perforator flaps]] |
||
* [[Mandible|Mandible reconstruction]] |
|||
* [[Rhinoplasty]] |
* [[Rhinoplasty]] |
||
* [[Rotation flap]] |
* [[Rotation flap]] |
||
* [[Skin cancer]] |
* [[Skin cancer]] |
||
* [[ |
* [[Z-plasty]] |
||
* [[z-plasty]] |
|||
==References== |
==References== |
||
{{Reflist|refs= |
{{Reflist|refs= |
||
<ref name="EssentialsForStudents"> |
<ref name="EssentialsForStudents"> |
||
{{cite book| vauthors = Song DH, Henry G, Reid RR, Wu LC, Wirth GA, Dorafshar AH| title = Plastic Surgery: Essentials for Students| chapter = Chapter 2: Grafts and Flaps| publisher = Plastic Surgery Education Foundation| year = 2007}}</ref> |
|||
{{cite book |
|||
<ref name="Guyuron8">{{cite book| vauthors = Guyuron B, Eriksson E, Persing JA| title = Plastic Surgery: Indications and Practice| publisher = Saunders Elsevier| year = 2009| volume = 1| chapter = Chapter 8: Flaps| isbn = 978-1-4160-4081-1}}</ref> |
|||
| first = David H. |
|||
<ref name="Guyuron9">{{cite book| vauthors = Guyuron B, Eriksson E, Persing JA| title = Plastic Surgery: Indications and Practice| publisher = Saunders Elsevier| year = 2009| volume = 1| chapter = Chapter 9: Microsurgery and Free Flaps| isbn = 978-1-4160-4081-1}}</ref> |
|||
| last = Song |
|||
<ref name="Erovic_2015">{{Cite book |vauthors = Erovic BM |url=http://worldcat.org/oclc/974391518 |title=Manual of Head and Neck Reconstruction Using Regional and Free Flaps |date=2015 |publisher=Springer Vienna |isbn=978-3-7091-1172-7 |oclc=974391518}}</ref> |
|||
|author2=Ginard Henry |author3=Russell R. Reid |author4=Liza C. Wu |author5=Garrett Wirth |author6=Amir H. Dorafshar |
|||
<ref name="Wolf_2011">{{Cite book |vauthors = Wolff KD, Hölzle F|url=https://www.worldcat.org/oclc/733542624 |title=Raising of microvascular flaps: a systematic approach |publisher=Springer |year=2011 |isbn=978-3-642-13831-7 |edition=2nd |location=Berlin |oclc=733542624}}</ref> |
|||
| title = Plastic Surgery: Essentials for Students |
|||
<ref name="Chung_2020">{{Cite book |vauthors = Chung KC|url=https://www.worldcat.org/oclc/1091585260 |title=Grabb and Smith's plastic surgery |date=2020 |isbn=978-1-4963-8824-7 |edition=8th |location=Philadelphia |oclc=1091585260}}</ref> |
|||
| chapter = Chapter 2: Grafts and Flaps |
|||
<ref name="Gillies_2019">{{Cite book |vauthors =Gillies HD |url=http://worldcat.org/oclc/1152260318 |title=Plastic Surgery of the Face Based on Selected Cases of War Injuries of the Face, Including Burns; With Original Illustrations |date=2019 |publisher=Forgotten Books |isbn=978-0-259-73591-5 |oclc=1152260318}}</ref> |
|||
| publisher = Plastic Surgery Education Foundation |
|||
<ref name="Guyuron8.2">{{Cite book |vauthors = Cormack GC, ((Lamberty BGH))|title= The arterial anatomy of skin flaps.|url=https://www.worldcat.org/oclc/12808179|location= London|publisher= Churchill Livingstone|year= 1986|oclc=12808179}}</ref> |
|||
| year = 2007 |
|||
<ref name="Carrau_2008">{{Cite book |last1=Carrau |first1=Ricardo L. |title=Chapter 105 - Reconstruction after Skull Base Surgery |date=2008-01-01 |url=https://www.sciencedirect.com/science/article/pii/B9781416024453501096 |work=Operative Otolaryngology: Head and Neck Surgery (Second Edition) |pages=1061–1068 |editor-last=Myers |editor-first=Eugene N. |place=Philadelphia |publisher=W.B. Saunders |language=en |isbn=978-1-4160-2445-3 |access-date=2022-10-30 |last2=Vescan |first2=Allan D. |last3=Snyderman |first3=Carl H. |last4=Kassam |first4=Amin B. |editor2-last=Carrau |editor2-first=Ricardo L. |editor3-last=Eibling |editor3-first=David E. |editor4-last=Ferguson |editor4-first=Berrylin J.}}</ref> |
|||
}}</ref> |
|||
<ref name="pmid13627972">{{cite journal | vauthors = Seidenberg B, Rosenak SS, Hurwitt ES, Som ML | title = Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment | journal = Ann Surg | volume = 149 | issue = 2 | pages = 162–71 | date = February 1959 | pmid = 13627972 | pmc = 1450976 | doi = 10.1097/00000658-195902000-00002 }}</ref> |
|||
<ref name="pmid24610608">{{cite journal | vauthors = Tomba P, Viganò A, Ruggieri P, Gasbarrini A | title = Gaspare Tagliacozzi, pioneer of plastic surgery and the spread of his technique throughout Europe in "De Curtorum Chirurgia per Insitionem" | journal = Eur Rev Med Pharmacol Sci | volume = 18 | issue = 4 | pages = 445–50 | date = 2014 | pmid = 24610608 }}</ref> |
|||
<ref name="Guyuron8"> |
|||
<ref name="pmid20431512">{{cite journal | vauthors = Chambers JA, Ray PD | title = Achieving growth and excellence in medicine: the case history of armed conflict and modern reconstructive surgery | journal = Ann Plast Surg | volume = 63 | issue = 5 | pages = 473–8 | date = November 2009 | pmid = 20431512 | doi = 10.1097/SAP.0b013e3181bc327a }}</ref> |
|||
{{cite book |
|||
<ref name="pmid6692066">{{cite journal | vauthors = Cormack GC, Lamberty BG | title = A classification of fascio-cutaneous flaps according to their patterns of vascularisation | journal = Br J Plast Surg | volume = 37 | issue = 1 | pages = 80–7 | date = January 1984 | pmid = 6692066 | doi = 10.1016/0007-1226(84)90049-3 }}</ref> |
|||
| first = Bahman |
|||
<ref name="pmid23190838">{{cite journal | vauthors = Saint-Cyr M, Wong C, Buchel EW, Colohan S, Pederson WC | title = Free tissue transfers and replantation | journal = Plast Reconstr Surg | volume = 130 | issue = 6 | pages = 858e–878e | date = December 2012 | pmid = 23190838 | doi = 10.1097/PRS.0b013e31826da2b7 | s2cid = 22788028 }}</ref> |
|||
| last = Guyuron |
|||
<ref name="pmid8942909">{{cite journal | vauthors = Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GR, Robb GL, Baldwin BJ | title = Timing of pedicle thrombosis and flap loss after free-tissue transfer | journal = Plast Reconstr Surg | volume = 98 | issue = 7 | pages = 1230–3 | date = December 1996 | pmid = 8942909 | doi = 10.1097/00006534-199612000-00017 | s2cid = 20380107 }}</ref> |
|||
|author2=Elof Eriksson |author3=John A. Persing |
|||
<ref name="pmid27556770">{{cite journal | vauthors = Buchanan PJ, Kung TA, Cederna PS | title = Evidence-Based Medicine: Wound Closure | journal = Plast Reconstr Surg | volume = 138 | issue = 3 Suppl | pages = 257S–270S | date = September 2016 | pmid = 27556770 | doi = 10.1097/PRS.0000000000002775 | s2cid = 5865301 }}</ref> |
|||
| title = Plastic Surgery: Indications and Practice |
|||
<ref name="pmid11735064">{{cite journal | vauthors = Clark JM, Wang TD | title = Local flaps in scar revision | journal = Facial Plast Surg | volume = 17 | issue = 4 | pages = 295–308 | date = November 2001 | pmid = 11735064 | doi = 10.1055/s-2001-18831 | s2cid = 42728956 }}</ref> |
|||
| publisher = Saunders Elsevier |
|||
<ref name="pmid10845282">{{cite journal | vauthors = Houseman ND, Taylor GI, Pan WR | title = The angiosomes of the head and neck: anatomic study and clinical applications | journal = Plast Reconstr Surg | volume = 105 | issue = 7 | pages = 2287–313 | date = June 2000 | pmid = 10845282 | doi = 10.1097/00006534-200006000-00001 | s2cid = 34422340 }}</ref> |
|||
| year = 2009 |
|||
<ref name="pmid15620622">{{cite journal | vauthors = Mellette JR, Ho DQ | title = Interpolation flaps | journal = Dermatol Clin | volume = 23 | issue = 1 | pages = 87–112, vi | date = January 2005 | pmid = 15620622 | doi = 10.1016/j.det.2004.08.010 }}</ref> |
|||
| volume = 1 |
|||
<ref name="pmid15814122">{{cite journal | vauthors = Tschoi M, Hoy EA, Granick MS | title = Skin flaps | journal = Clin Plast Surg | volume = 32 | issue = 2 | pages = 261–73 | date = April 2005 | pmid = 15814122 | doi = 10.1016/j.cps.2004.11.005 }}</ref> |
|||
| chapter = Chapter 8: Flaps |
|||
<ref name="pmid16816714">{{cite journal | vauthors = Turner AJ, Parkhouse N | title = Revisiting the reconstructive ladder | journal = Plast Reconstr Surg | volume = 118 | issue = 1 | pages = 267–8 | date = July 2006 | pmid = 16816714 | doi = 10.1097/01.prs.0000222224.03137.d5 }}</ref> |
|||
| isbn = 978-1-4160-4081-1 |
|||
<ref name="pmid7661898">{{cite journal | vauthors = Gottlieb LJ, Krieger LM | title = From the reconstructive ladder to the reconstructive elevator | journal = Plast Reconstr Surg | volume = 93 | issue = 7 | pages = 1503–4 | date = June 1994 | pmid = 7661898 | doi = 10.1097/00006534-199406000-00027 | doi-access = free }}</ref> |
|||
}}</ref> |
|||
<ref name="pmid16565127">{{cite journal | vauthors = Boyce DE, Shokrollahi K | title = Reconstructive surgery | journal = BMJ | volume = 332 | issue = 7543 | pages = 710–2 | date = March 2006 | pmid = 16565127 | pmc = 1410906 | doi = 10.1136/bmj.332.7543.710 }}</ref> |
|||
<ref name="pmid3567445">{{cite journal | vauthors = Taylor GI, Palmer JH | title = The vascular territories (angiosomes) of the body: experimental study and clinical applications | journal = Br J Plast Surg | volume = 40 | issue = 2 | pages = 113–41 | date = March 1987 | pmid = 3567445 | doi = 10.1016/0007-1226(87)90185-8 }}</ref> |
|||
<ref name="Guyuron9"> |
|||
{{cite book |
|||
| first = Bahman |
|||
| last = Guyuron |
|||
|author2=Elof Eriksson |author3=John A. Persing |
|||
| title = Plastic Surgery: Indications and Practice |
|||
| publisher = Saunders Elsevier |
|||
| year = 2009 |
|||
| volume = 1 |
|||
| chapter = Chapter 9: Microsurgery and Free Flaps |
|||
| isbn = 978-1-4160-4081-1 |
|||
}}</ref> |
|||
<ref name="Guyuron8.2">Cormack GC, Lamberty BGH. The arterial anatomy of skin flaps. London: Churchill Livingstone; 1986.</ref> |
|||
<ref name="Guyuron8.3">Clark JM, Wang TD. Local flaps in scar revision. Facial Plast Surg 2001; 17(4):295–308.</ref> |
|||
<ref name="Guyuron8.5">Houseman ND, Taylor GI, Pan WR. The angiosomes of the head and neck: anatomic study and clinical applications. Plast Reconstr Surg. 2000; 105(7):2287–2313.</ref> |
|||
<ref name="Guyuron8.23">Turner AJ, Parkhouse N. Revisiting the reconstructive ladder. Plast Reconst Surg 2006; 118(1):267–268.</ref> |
|||
<ref name="Guyuron8.38">Mellette JR, Ho DQ. Interpolation flaps. Dermatol Clin 2005; 23(1):87–112.</ref> |
|||
<ref name="Guyuron8.41">Tschoi M, Hoy FA, Granick MS. Skin flaps. Clin Plast Surg 2005; 32(2):261–273.</ref> |
|||
}} |
}} |
||
Latest revision as of 17:49, 28 June 2024
| Flap surgery | |
|---|---|
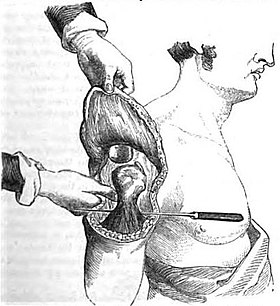 Engraving by John Eric Erichsen depicting flap surgery used to cover an amputation stump | |
| ICD-9-CM | 86.7 |
Flap surgery is a technique in plastic and reconstructive surgery where tissue with an intact blood supply is lifted from a donor site and moved to a recipient site. Flaps are distinct from grafts, which do not have an intact blood supply and relies on the growth of new blood vessels. Flaps are done to fill a defect such as a wound resulting from injury or surgery when the remaining tissue is unable to support a graft, or to rebuild more complex anatomic structures like breasts or jaws.[1][2]
Uses
[edit]Flap surgery is a technique essential to plastic and reconstructive surgery. A flap is defined as tissue that can be moved to another site and has its own blood supply. This is in comparison to a skin graft which does not have its own blood supply and relies on vascularization from the recipient site.[2] Flaps have many uses in wound healing and are used when wounds are large, complex, or need tissue and bulk for successful closure.[2]
Anatomy
[edit]Flaps can contain many different combination of layers of tissue, from skin to bone (see § Classification). The main goal of a flap is to maintain blood flow to tissue to maintain survival, and understanding the anatomy in flap design is key to a successful flap surgery.[2]

Skin anatomy
[edit]Flaps may include skin in their construction. Skin is important for many reasons, but namely its role in thermoregulation, immune function, and blood supply aid in flap survival.[2] The skin can be divided into three main layers: the epidermis, dermis, and subcutaneous tissue. Blood is mainly supplied to the skin by two networks of blood vessels. The deep network lies between the dermis and the subcutaneous tissue, while the shallow network lies within the papillary layer of the dermis.[3] The epidermis is supplied by diffusion from this shallow network and both networks are supplied by collaterals, and by perforating arteries that bring blood from deeper layers either between muscles (septocutaneous perforators) or through muscles (musculocutaneous perforators).[2]
This robust and redundant blood supply is important in flap surgery,[2] because flaps are cut off from other blood vessels when it is raised and removed from its surrounding native tissue.[2] The remaining blood supply must then keep the tissue alive until additional blood supply can be formed through angiogenesis.[4]
Angiosome
[edit]The angiosome is a concept first coined by Ian Taylor in 1987.[5] It is a three-dimensional region of tissue that is supplied by a single artery and can include skin, soft tissue, and bone.[5][6] Adjacent angiosomes are connected by narrower choke vessels, and multiple angiosomes can be supplied by a single artery. Knowledge of these supply arteries and their associated angiosomes is useful in planning the location, size, and shape of a flap.[4]
Classification
[edit]Flaps can be fundamentally classified by their mechanism of movement, the types of tissues present, or by their blood supply.[2] The surgeon generally chooses the least complex type that will achieve the desired effect via a concept known as the reconstructive ladder.[7][8]
Mechanism of movement
[edit]- Local flaps are created by freeing a layer of tissue and then stretching the freed layer to fill a defect. This is the least complex type of flap and includes advancement flaps, rotation flaps, and transposition flaps, in order from least to most complex. With an advancement flap, incisions are extended out parallel from the wound, creating a rectangle with one edge remaining intact. This rectangle is freed from the deeper tissues and then stretched (or advanced) forward to cover the wound. The flap is disconnected from the body except for the uncut edge which contains the blood supply which feeds in horizontally. A rotation flap is similar except instead of being stretched in a straight line, the flap is stretched in an arc. The more complex transposition flap involves rotating an adjacent piece of tissue, resulting in the creation of a new defect that must then be closed.[4]
- Regional or interpolation flaps are not immediately adjacent to the defect. Instead, the freed tissue "island" is moved over or underneath normal tissue to reach the defect to be filled, with the blood supply still connected to the donor site via a pedicle.[9] The pedicle can be removed after a new blood supply has formed. Examples: pectoralis major myocutaneous flap and deltopectoral flap for head and neck defects, and latissimus dorsi flap and traverse rectus abdominal muscle (TRAM) flap for breast reconstruction.[4]
- Distant flaps are used when the donor site is far from the defect. These are the most complex class of flap. Direct or tubed flaps involve having the flap connected to both the donor and recipient sites simultaneously, forming a bridge. This allows blood to be supplied by the donor site while a new blood supply from the recipient site is formed. Once this happens, the bridge can be disconnected from the donor site if necessary, completing the transfer.[10] A free flap has the blood supply cut and then reattached microsurgically to a new blood supply at the recipient site.[11][12]
Tissue type
[edit]Flaps can be classified by the content of the tissue within them.
- Cutaneous flaps contain the full thickness of the skin, fat, and superficial fascia and are used to fill small defects. These are typically supplied by a random blood supply. Examples include Z-plasty, deep inferior epigastric perforator (DIEP) flaps, and V-Y advancement flaps.[2]
- Fasciocutaneous flaps contain subcutaneous tissue and deep fascia, resulting in a more robust blood supply and ability to fill a larger defect. The Cormack and Lamberty classification is used for the vascular supply of faciocutaneous flaps.[13] Examples: temporoparietal and anterolateral thigh fascocutaneous flap, lateral fasciocutaneous flap, posterior fasciocutaneous flap.[2]

- Musculocutaneous and muscle flaps contain a layer of muscle to provide bulk that can fill a deeper defect. If skin cover is needed, a skin graft can be placed over top of it. Examples: gastrocnemius flap, latissimus dorsi flap, TRAM flap, and transverse upper gracillis flap.[2]
- Bone flaps contain bone and are used when structural support is needed such as in jaw reconstruction. Example: fibula flap.[2][4][14]
- Omental flaps can be used in chest wall defects, and intestinal flaps can be used to reconstruct tubular structures like the esophagus.[2]
Vascular supply
[edit]Classification based on blood supply to the flap:
- Axial flaps are supplied by a named artery and vein. This allows for a larger area to be freed from surrounding and underlying tissue, leaving only a small pedicle containing the vessels.[2] Reverse-flow flaps are a type of axial flap in which the supply artery is cut on one end and blood is supplied by backwards flow from the other direction. Random flaps are simpler and have no named blood supply; they are supplied by the subdermal plexus.[3][4]
- Pedicled flaps remain attached to the donor site via a pedicle that contains the blood supply, in contrast to a free flap, where the vessels are cut and anastomosed to another blood supply.[1][2]
Contraindications
[edit]Anyone who is unstable for surgery should not undergo flap surgery. As with most surgeries, people who are sicker may have more difficulties with wound healing, which include individuals with comorbidities such as diabetes, smoking, immunosuppression, and vascular disease.[15][16]
Risks or complications
[edit]The risks of flap surgery include infection, wound breakdown, fluid accumulation, bleeding, damage to nearby structures, and scarring.[10] The most notable risk in this procedure is flap death, where the flap loses blood supply. The loss of blood can be due to many reasons, but is commonly due to tension on the vascular supply and insufficient blood flow to the end segments of the flap.[10] This can sometimes be fixed with another surgery or using additional methods of healing in the reconstructive ladder.[17]
Recovery
[edit]As with healing of any wound, healing of a flap maintains the same process of wound healing. There are four stages to wound healing: hemostasis, inflammation, proliferation, and remodeling, all of which can take up to a year to complete.[18][2]
Following flap surgery, the biggest risk in recovery is flap death. Flap failure is an uncommon occurrence but does happen. The reported flap failure rate in free flaps is less than 5%.[19] The most commonly cause is by venous insufficiency consisting of 54% of all causes.[19] Venous insufficiency is commonly caused by a venous thrombus within the first 2 days following surgery.[19][18] After the immediate postoperative risk, the flap will continue to heal adhering to the stages of normal wound healing and will take over 3 months for an incision to be at 80% tensile strength compared to normal tissue.[18]

History
[edit]Skin flaps are an essential part of a surgeon's toolbox in plastic surgery. It is part of the reconstructive ladder.[17] The first known reports of surgical flaps originated in 600 BC in India by Sushruta where the tilemakers' caste would reconstruct noses using regional flaps due to the practice of nose amputations as a form of legal punishment.[20][17] The next description of flap surgery comes from Celsus, an ancient Roman who described the advancement of skin flaps from 25 BC to 50 AD.[20][17] In the 15th century, Gaspare Tagliacozzi, an Italian surgeon, helped develop the "Italian method" for nasal reconstruction, a delayed pedicle skin graft, where the skin from the arm would be attached to the nose for many months to create the reconstruction, first printed in the 1597 book De Curtorum Chirurgia per Insitionem.[21] The Italian method was rediscovered in 1800 by German surgeon Carl Ferdinand von Graefe.[22] Major advancements in modern plastic surgery are mostly attributed to Harold Gillies, who pioneered facial reconstruction during World War I using pedicled tube flaps on patients like Walter Yeo, and the development of the walking-stalk skin flap by Gilles' cousin Archibald McIndoe in 1930.[20][23]
Advancements continued in flap surgery. With the introduction of the operating microscope, microvascular surgery advancements allowed for the anastomosis of blood vessels.[12] This led to the ability of free tissue transfers, and in 1958 Bernard Seidenberg transferred a part of the jejunum to the esophagus to remove a cancer.[12][24] Modern advancements in flap surgeries have continued since this time and are now commonly used in many procedures.[12]
See also
[edit]- Breast reconstruction
- DIEP flap
- Hand surgery
- List of plastic surgery flaps
- Perforator flaps
- Rhinoplasty
- Rotation flap
- Skin cancer
- Z-plasty
References
[edit]- ^ a b Song DH, Henry G, Reid RR, Wu LC, Wirth GA, Dorafshar AH (2007). "Chapter 2: Grafts and Flaps". Plastic Surgery: Essentials for Students. Plastic Surgery Education Foundation.
- ^ a b c d e f g h i j k l m n o p q Chung KC (2020). Grabb and Smith's plastic surgery (8th ed.). Philadelphia. ISBN 978-1-4963-8824-7. OCLC 1091585260.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ a b Clark JM, Wang TD (November 2001). "Local flaps in scar revision". Facial Plast Surg. 17 (4): 295–308. doi:10.1055/s-2001-18831. PMID 11735064. S2CID 42728956.
- ^ a b c d e f Guyuron B, Eriksson E, Persing JA (2009). "Chapter 8: Flaps". Plastic Surgery: Indications and Practice. Vol. 1. Saunders Elsevier. ISBN 978-1-4160-4081-1.
- ^ a b Taylor GI, Palmer JH (March 1987). "The vascular territories (angiosomes) of the body: experimental study and clinical applications". Br J Plast Surg. 40 (2): 113–41. doi:10.1016/0007-1226(87)90185-8. PMID 3567445.
- ^ Houseman ND, Taylor GI, Pan WR (June 2000). "The angiosomes of the head and neck: anatomic study and clinical applications". Plast Reconstr Surg. 105 (7): 2287–313. doi:10.1097/00006534-200006000-00001. PMID 10845282. S2CID 34422340.
- ^ Turner AJ, Parkhouse N (July 2006). "Revisiting the reconstructive ladder". Plast Reconstr Surg. 118 (1): 267–8. doi:10.1097/01.prs.0000222224.03137.d5. PMID 16816714.
- ^ Boyce DE, Shokrollahi K (March 2006). "Reconstructive surgery". BMJ. 332 (7543): 710–2. doi:10.1136/bmj.332.7543.710. PMC 1410906. PMID 16565127.
- ^ Mellette JR, Ho DQ (January 2005). "Interpolation flaps". Dermatol Clin. 23 (1): 87–112, vi. doi:10.1016/j.det.2004.08.010. PMID 15620622.
- ^ a b c Tschoi M, Hoy EA, Granick MS (April 2005). "Skin flaps". Clin Plast Surg. 32 (2): 261–73. doi:10.1016/j.cps.2004.11.005. PMID 15814122.
- ^ Guyuron B, Eriksson E, Persing JA (2009). "Chapter 9: Microsurgery and Free Flaps". Plastic Surgery: Indications and Practice. Vol. 1. Saunders Elsevier. ISBN 978-1-4160-4081-1.
- ^ a b c d Wolff KD, Hölzle F (2011). Raising of microvascular flaps: a systematic approach (2nd ed.). Berlin: Springer. ISBN 978-3-642-13831-7. OCLC 733542624.
- ^ Cormack GC, Lamberty BG (January 1984). "A classification of fascio-cutaneous flaps according to their patterns of vascularisation". Br J Plast Surg. 37 (1): 80–7. doi:10.1016/0007-1226(84)90049-3. PMID 6692066.
- ^ Cormack GC, Lamberty BGH (1986). The arterial anatomy of skin flaps. London: Churchill Livingstone. OCLC 12808179.
- ^ Carrau, Ricardo L.; Vescan, Allan D.; Snyderman, Carl H.; Kassam, Amin B. (2008-01-01). Myers, Eugene N.; Carrau, Ricardo L.; Eibling, David E.; Ferguson, Berrylin J. (eds.). Chapter 105 - Reconstruction after Skull Base Surgery. Philadelphia: W.B. Saunders. pp. 1061–1068. ISBN 978-1-4160-2445-3. Retrieved 2022-10-30.
{{cite book}}:|work=ignored (help) - ^ Saint-Cyr M, Wong C, Buchel EW, Colohan S, Pederson WC (December 2012). "Free tissue transfers and replantation". Plast Reconstr Surg. 130 (6): 858e–878e. doi:10.1097/PRS.0b013e31826da2b7. PMID 23190838. S2CID 22788028.
- ^ a b c d Gottlieb LJ, Krieger LM (June 1994). "From the reconstructive ladder to the reconstructive elevator". Plast Reconstr Surg. 93 (7): 1503–4. doi:10.1097/00006534-199406000-00027. PMID 7661898.
- ^ a b c Buchanan PJ, Kung TA, Cederna PS (September 2016). "Evidence-Based Medicine: Wound Closure". Plast Reconstr Surg. 138 (3 Suppl): 257S–270S. doi:10.1097/PRS.0000000000002775. PMID 27556770. S2CID 5865301.
- ^ a b c Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GR, Robb GL, Baldwin BJ (December 1996). "Timing of pedicle thrombosis and flap loss after free-tissue transfer". Plast Reconstr Surg. 98 (7): 1230–3. doi:10.1097/00006534-199612000-00017. PMID 8942909. S2CID 20380107.
- ^ a b c Chambers JA, Ray PD (November 2009). "Achieving growth and excellence in medicine: the case history of armed conflict and modern reconstructive surgery". Ann Plast Surg. 63 (5): 473–8. doi:10.1097/SAP.0b013e3181bc327a. PMID 20431512.
- ^ Tomba P, Viganò A, Ruggieri P, Gasbarrini A (2014). "Gaspare Tagliacozzi, pioneer of plastic surgery and the spread of his technique throughout Europe in "De Curtorum Chirurgia per Insitionem"". Eur Rev Med Pharmacol Sci. 18 (4): 445–50. PMID 24610608.
- ^ Erovic BM (2015). Manual of Head and Neck Reconstruction Using Regional and Free Flaps. Springer Vienna. ISBN 978-3-7091-1172-7. OCLC 974391518.
- ^ Gillies HD (2019). Plastic Surgery of the Face Based on Selected Cases of War Injuries of the Face, Including Burns; With Original Illustrations. Forgotten Books. ISBN 978-0-259-73591-5. OCLC 1152260318.
- ^ Seidenberg B, Rosenak SS, Hurwitt ES, Som ML (February 1959). "Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment". Ann Surg. 149 (2): 162–71. doi:10.1097/00000658-195902000-00002. PMC 1450976. PMID 13627972.



