Glandular odontogenic cyst: Difference between revisions
No edit summary |
No edit summary |
||
| Line 27: | Line 27: | ||
}} |
}} |
||
A '''glandular odontogenic cyst''' is a rare and [[Benign tumor|benign]] [[odontogenic cyst]] developed at the odontogenic epithelium of the [[mandible]] or [[maxilla]].<ref name=pmid26587384>{{cite journal |last1=Faisal |first1=Mohammad |last2=Ahmad |first2=Syed Ansar |last3=Ansari |first3=Uzma |title=Glandular odontogenic cyst – Literature review and report of a paediatric case |journal=Journal of Oral Biology and Craniofacial Research |date=September 2015 |volume=5 |issue=3 |pages=219–225 |doi=10.1016/j.jobcr.2015.06.011 |pmid=26587384 |pmc=4623883 }}</ref><ref name=pmid21180452>{{cite journal |last1=Prabhu |first1=Sudeendra |last2=Rekha |first2=K |last3=Kumar |first3=GS |title=Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma |journal=Journal of Oral and Maxillofacial Pathology |date=2010 |volume=14 |issue=1 |pages=12–5 |doi=10.4103/0973-029X.64303 |pmid=21180452 |pmc=2996005 }}</ref><ref name=pmid24374982>{{cite journal |last1=Motooka |first1=Naomi |last2=Ohba |first2=Seigo |last3=Uehara |first3=Masataka |last4=Fujita |first4=Syuichi |last5=Asahina |first5=Izumi |title=A case of glandular odontogenic cyst in the mandible treated with the dredging method |journal=Odontology |date=1 January 2015 |volume=103 |issue=1 |pages=112–115 |doi=10.1007/s10266-013-0143-0 |pmid=24374982 |s2cid=21059170 }}</ref><ref name=pmid27134453>{{cite journal |last1=Shah |first1=AmishaA |last2=Sangle |first2=Amit |last3=Bussari |first3=Smita |last4=Koshy |first4=AjitV |title=Glandular odontogenic cyst: A diagnostic dilemma |journal=Indian Journal of Dentistry |date=2016 |volume=7 |issue=1 |pages=38–43 |doi=10.4103/0975-962X.179371 |pmid=27134453 |pmc=4836096 }}</ref> Originally, the cyst was labeled as 'sialo-odontogenic cyst' in 1987.<ref name="Shear & Speight 2007">{{cite book |doi=10.1002/9780470759769.ch7 |chapter=Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst) |title=Cysts of the Oral and Maxillofacial Regions |year=2007 |
A '''glandular odontogenic cyst''' is a rare and [[Benign tumor|benign]] [[odontogenic cyst]] developed at the odontogenic epithelium of the [[mandible]] or [[maxilla]].<ref name=pmid26587384>{{cite journal |last1=Faisal |first1=Mohammad |last2=Ahmad |first2=Syed Ansar |last3=Ansari |first3=Uzma |title=Glandular odontogenic cyst – Literature review and report of a paediatric case |journal=Journal of Oral Biology and Craniofacial Research |date=September 2015 |volume=5 |issue=3 |pages=219–225 |doi=10.1016/j.jobcr.2015.06.011 |pmid=26587384 |pmc=4623883 }}</ref><ref name=pmid21180452>{{cite journal |last1=Prabhu |first1=Sudeendra |last2=Rekha |first2=K |last3=Kumar |first3=GS |title=Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma |journal=Journal of Oral and Maxillofacial Pathology |date=2010 |volume=14 |issue=1 |pages=12–5 |doi=10.4103/0973-029X.64303 |pmid=21180452 |pmc=2996005 }}</ref><ref name=pmid24374982>{{cite journal |last1=Motooka |first1=Naomi |last2=Ohba |first2=Seigo |last3=Uehara |first3=Masataka |last4=Fujita |first4=Syuichi |last5=Asahina |first5=Izumi |title=A case of glandular odontogenic cyst in the mandible treated with the dredging method |journal=Odontology |date=1 January 2015 |volume=103 |issue=1 |pages=112–115 |doi=10.1007/s10266-013-0143-0 |pmid=24374982 |s2cid=21059170 }}</ref><ref name=pmid27134453>{{cite journal |last1=Shah |first1=AmishaA |last2=Sangle |first2=Amit |last3=Bussari |first3=Smita |last4=Koshy |first4=AjitV |title=Glandular odontogenic cyst: A diagnostic dilemma |journal=Indian Journal of Dentistry |date=2016 |volume=7 |issue=1 |pages=38–43 |doi=10.4103/0975-962X.179371 |pmid=27134453 |pmc=4836096 }}</ref> Originally, the cyst was labeled as 'sialo-odontogenic cyst' in 1987.<ref name="Shear & Speight 2007">{{cite book |doi=10.1002/9780470759769.ch7 |chapter=Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst) |pages=94–99 |chapterurl=https://books.google.com/books?id=Jgt7046OlUAC&pg=PA94 |editor1-last=Shear |editor1-first=Mervyn |editor2-last=Speight |editor2-first=Paul |title=Cysts of the Oral and Maxillofacial Regions |year=2007 |isbn=978-0-470-75976-9 }}</ref> However, the [[World Health Organisation]] (WHO) decided to adopt the medical expression 'glandular odontogenic cyst'.<ref name=pmid24374982/> Following the initial classification, only 60 medically documented cases were present in the population by 2003.<ref name=pmid15789313>{{cite journal |last1=Kaplan |first1=Ilana |last2=Gal |first2=Gavriel |last3=Anavi |first3=Yakir |last4=Manor |first4=Ronen |last5=Calderon |first5=Shlomo |title=Glandular odontogenic cyst: Treatment and recurrence |journal=Journal of Oral and Maxillofacial Surgery |date=April 2005 |volume=63 |issue=4 |pages=435–441 |doi=10.1016/j.joms.2004.08.007 |pmid=15789313 }}</ref> It was established as its own biological growth after differentiation from other jaw cysts such as the ‘central mucoepidermoid carcinoma’, a popular type of neoplasm at the salivary glands.<ref name="Shear & Speight 2007"/><ref name=pmid29131467>{{cite journal |last1=Nagasaki |first1=Atsuhiro |last2=Ogawa |first2=Ikuko |last3=Sato |first3=Yukiko |last4=Takeuchi |first4=Kengo |last5=Kitagawa |first5=Masae |last6=Ando |first6=Toshinori |last7=Sakamoto |first7=Shinnichi |last8=Shrestha |first8=Madhu |last9=Uchisako |first9=Kaori |last10=Koizumi |first10=Koichi |last11=Toratani |first11=Shigeaki |last12=Konishi |first12=Masaru |last13=Takata |first13=Takashi |title=Central mucoepidermoid carcinoma arising from glandular odontogenic cyst confirmed by analysis of MAML2 rearrangement: A case report: Central MEC arising from GOC |journal=Pathology International |date=January 2018 |volume=68 |issue=1 |pages=31–35 |doi=10.1111/pin.12609 |pmid=29131467 |s2cid=8932602 }}</ref> The cyst is usually misdiagnosed with other lesions developed at the glandular and [[salivary gland]] due to the shared clinical signs.<ref name=pmid27829208>{{cite journal |last1=AbdullGaffar |first1=Badr |last2=Koilelat |first2=Mohamed |title=Glandular Odontogenic Cyst: The Value of Intraepithelial Hemosiderin |journal=International Journal of Surgical Pathology |date=May 2017 |volume=25 |issue=3 |pages=250–252 |doi=10.1177/1066896916672333 |pmid=27829208 |s2cid=46588216 }}</ref> This odontogenic cyst is commonly described to be a slow and aggressive development.<ref name=pmid25848155>{{cite journal |last1=Akkaş |first1=İsmail |last2=Toptaş |first2=Orçun |last3=Özan |first3=Fatih |last4=Yılmaz |first4=Fahri |title=Bilateral Glandular Odontogenic Cyst of Mandible: A Rare Occurrence |journal=Journal of Maxillofacial and Oral Surgery |date=1 March 2015 |volume=14 |issue=1 |pages=443–447 |doi=10.1007/s12663-014-0668-y |pmid=25848155 |pmc=4379287 }}</ref> The inclination of the cyst to be large and multilocular is associated with a greater chance of remission.<ref name=pmid25971944>{{cite journal |last1=Momeni Roochi |first1=Mehrnoush |last2=Tavakoli |first2=Iman |last3=Ghazi |first3=Fatemeh Mojgan |last4=Tavakoli |first4=Ali |title=Case series and review of glandular odontogenic cyst with emphasis on treatment modalities |journal=Journal of Cranio-Maxillofacial Surgery |date=1 July 2015 |volume=43 |issue=6 |pages=746–750 |doi=10.1016/j.jcms.2015.03.030 |pmid=25971944 }}</ref><ref name=pmid27134453/> The cyst is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases.<ref name=Neville2016>{{cite book |doi=10.1007/978-3-319-28085-1_677 |chapter=Cyst, Glandular Odontogenic |title=Encyclopedia of Soil Science |series=Encyclopedia of Earth Sciences Series |year=2016 |last1=Neville |first1=Brad W. |pages=89–93 |isbn=978-1-4020-3994-2 }}</ref> Reported cases show that the cyst mainly impacts the mandible and male individuals.<ref name=pmid25971944/> The presentation of the cyst to be at the maxilla has a very low rate of incidence.<ref name=pmid21180452/> It is more common in adults in their fifth and sixth decades.<ref name="Borges et al 2012"/> |
||
The cyst has signs and symptoms of varying sensitivities, and dysfunction.<ref name=Neville2016/><ref name=pmid25848155/> In some cases, the cyst will present no common abnormalities and remains undiagnosed until secondary complications arise.<ref name=pmid25848155/> The proliferation of cyst requires insight into its unique histochemistry.<ref name="Shear & Speight 2007"/> The comparable characteristics of the cyst with other jaw lesions require physicians to closely examine the histology, morphology, and immunocytochemistry for a differential diagnosis.<ref name=pmid27134453/> Treatment modes of the cyst follow a case-by-case approach due to its variable nature.<ref name=pmid21865053>{{cite journal |last1=Cano |first1=Jorge |last2=Benito |first2=Dulce María |last3=Montáns |first3=José |last4=Rodríguez-Vázquez |first4=José Francisco |last5=Campo |first5=Julián |last6=Colmenero |first6=César |title=Glandular odontogenic cyst: Two high-risk cases treated with conservative approaches |journal=Journal of Cranio-Maxillofacial Surgery |date=1 July 2012 |volume=40 |issue=5 |pages=e131–e136 |doi=10.1016/j.jcms.2011.07.005 |pmid=21865053 }}</ref> The selected treatment must have an appropriate pre and post-operative plan.<ref name=pmid21865053/> |
The cyst has signs and symptoms of varying sensitivities, and dysfunction.<ref name=Neville2016/><ref name=pmid25848155/> In some cases, the cyst will present no common abnormalities and remains undiagnosed until secondary complications arise.<ref name=pmid25848155/> The proliferation of cyst requires insight into its unique histochemistry.<ref name="Shear & Speight 2007"/> The comparable characteristics of the cyst with other jaw lesions require physicians to closely examine the histology, morphology, and immunocytochemistry for a differential diagnosis.<ref name=pmid27134453/> Treatment modes of the cyst follow a case-by-case approach due to its variable nature.<ref name=pmid21865053>{{cite journal |last1=Cano |first1=Jorge |last2=Benito |first2=Dulce María |last3=Montáns |first3=José |last4=Rodríguez-Vázquez |first4=José Francisco |last5=Campo |first5=Julián |last6=Colmenero |first6=César |title=Glandular odontogenic cyst: Two high-risk cases treated with conservative approaches |journal=Journal of Cranio-Maxillofacial Surgery |date=1 July 2012 |volume=40 |issue=5 |pages=e131–e136 |doi=10.1016/j.jcms.2011.07.005 |pmid=21865053 }}</ref> The selected treatment must have an appropriate pre and post-operative plan.<ref name=pmid21865053/> |
||
| Line 89: | Line 89: | ||
* {{cite journal |last1=Patel |first1=Govind |last2=Shah |first2=Monali |last3=Kale |first3=Hemant |last4=Ranginwala |first4=Amena |title=Glandular odontogenic cyst: A rare entity |journal=Journal of Oral and Maxillofacial Pathology |date=2014 |volume=18 |issue=1 |pages=89 |doi=10.4103/0973-029X.131922 |pmid=24959044 |pmc=4065455 }} |
* {{cite journal |last1=Patel |first1=Govind |last2=Shah |first2=Monali |last3=Kale |first3=Hemant |last4=Ranginwala |first4=Amena |title=Glandular odontogenic cyst: A rare entity |journal=Journal of Oral and Maxillofacial Pathology |date=2014 |volume=18 |issue=1 |pages=89 |doi=10.4103/0973-029X.131922 |pmid=24959044 |pmc=4065455 }} |
||
* {{cite journal |last1=Shah |first1=AmishaA |last2=Sangle |first2=Amit |last3=Bussari |first3=Smita |last4=Koshy |first4=AjitV |title=Glandular odontogenic cyst: A diagnostic dilemma |journal=Indian Journal of Dentistry |date=2016 |volume=7 |issue=1 |pages=38–43 |doi=10.4103/0975-962X.179371 |pmid=27134453 |pmc=4836096 }} |
* {{cite journal |last1=Shah |first1=AmishaA |last2=Sangle |first2=Amit |last3=Bussari |first3=Smita |last4=Koshy |first4=AjitV |title=Glandular odontogenic cyst: A diagnostic dilemma |journal=Indian Journal of Dentistry |date=2016 |volume=7 |issue=1 |pages=38–43 |doi=10.4103/0975-962X.179371 |pmid=27134453 |pmc=4836096 }} |
||
* {{cite book |doi=10.1002/9780470759769.ch7 |chapter=Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst) |title=Cysts of the Oral and Maxillofacial Regions |year=2007 |
* {{cite book |doi=10.1002/9780470759769.ch7 |chapter=Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst) |pages=94–99 |chapterurl=https://books.google.com/books?id=Jgt7046OlUAC&pg=PA94 |editor1-last=Shear |editor1-first=Mervyn |editor2-last=Speight |editor2-first=Paul |title=Cysts of the Oral and Maxillofacial Regions |year=2007 |isbn=978-0-470-75976-9 }} |
||
Revision as of 18:20, 19 November 2020
| Glandular odontogenic cyst | |
|---|---|
| Other names | Sialo-Odontogenic cyst |
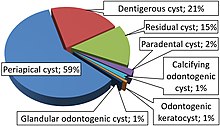 | |
| Relative incidence of odontogenic cysts.[1] Glandular odontogenic cyst is labeled at bottom. | |
| Symptoms | Expansion of the jaw, swelling, impairment to tooth, root and cortical plate [2][3] |
| Causes | Cellular mutation, cyst maturation at glandular, BCL-2 protein [2][4] |
| Differential diagnosis | Central mucoepidermoid carcinoma, odontogenic keratocyst [5][6] |
| Treatment | Enucleation, curettage, marginal or partial resection, marsupialization[6] |
| Frequency | 0.12 to 0.13% of people [2] |
A glandular odontogenic cyst is a rare and benign odontogenic cyst developed at the odontogenic epithelium of the mandible or maxilla.[2][7][8][9] Originally, the cyst was labeled as 'sialo-odontogenic cyst' in 1987.[5] However, the World Health Organisation (WHO) decided to adopt the medical expression 'glandular odontogenic cyst'.[8] Following the initial classification, only 60 medically documented cases were present in the population by 2003.[6] It was established as its own biological growth after differentiation from other jaw cysts such as the ‘central mucoepidermoid carcinoma’, a popular type of neoplasm at the salivary glands.[5][10] The cyst is usually misdiagnosed with other lesions developed at the glandular and salivary gland due to the shared clinical signs.[11] This odontogenic cyst is commonly described to be a slow and aggressive development.[12] The inclination of the cyst to be large and multilocular is associated with a greater chance of remission.[3][9] The cyst is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases.[13] Reported cases show that the cyst mainly impacts the mandible and male individuals.[3] The presentation of the cyst to be at the maxilla has a very low rate of incidence.[7] It is more common in adults in their fifth and sixth decades.[1]
The cyst has signs and symptoms of varying sensitivities, and dysfunction.[13][12] In some cases, the cyst will present no common abnormalities and remains undiagnosed until secondary complications arise.[12] The proliferation of cyst requires insight into its unique histochemistry.[5] The comparable characteristics of the cyst with other jaw lesions require physicians to closely examine the histology, morphology, and immunocytochemistry for a differential diagnosis.[9] Treatment modes of the cyst follow a case-by-case approach due to its variable nature.[14] The selected treatment must have an appropriate pre and post-operative plan.[14]
Signs and Symptoms
The appearance of a protrusive growth will be present at their mandible or maxilla.[2] The expansive nature of this cyst may destruct the quality of symmetry at the facial region and would be a clear physical sign of abnormality.[2][5] The area of impact will likely be at the anterior region of mandible due its presence in a significant amount reported cases.[7] A painful and swollen sensation at the jaw region caused by the cystic growth has been described.[13] Detailing of a painless feeling or facial paraesthesia can be possible.[13][5] Alongside the growth, "root resorption, cortical bone thinning and perforation, and tooth displacement may occur".[3] Experience of swelling at the buccal and lingual zones can occur.[6] Usually, the smaller sized cysts present no signs or symptoms to the case.[4] The cyst can begin its proliferation at the anterior region of the teeth and eventually mediate expansion at the molars.[5] The lesion is filled with cystic a fluid that differs in viscosity and may appear as transparent, brownish-red, or creamy in colour.[3]
Causes

The origin of this cyst can be understood through its biological and histopathlogical foundations.[4] It has been suggested that the occurrence of the cyst is a result of a traumatic event.[11] The occurrence of this cyst may be from a mutated cell from "the oral mucosa and the dental follicle" origin.[15] Another probable cause is from pre-existing cysts or cancerous constituents.[11] A potential biological origin is a cyst developed at a salivary gland or simple epithelium, which then matures at the tissue of the glandular.[4] Another origin is when a primordial cyst infiltrates the glandular epithelial tissue through a highly organised cellular differentiation.[4] Also, it can arise from a singular cystic space induced by a cancerous mass.[4] Pathologists discovered a BCL-2 protein that is commonly present in neoplasms, to exist in the tissue layers of the cyst.[4][15] The protein is capable of disrupting normal cell death function at the odontogenic region.[4][15] The analysis of PTCH, a gene that specialises in neoplasm inhibition, was carried out to determine if any existing mutations played a role in the initiation of the glandular odontogenic cyst.[5] It is confirmed that the gene has no assistance in triggering cystic advancement.[5]
Diagnosis
Radiology
The performance of computed tomography at the area of impact is essential.[12] Radiographic imaging of the cyst can display a defined unilocular or multilocular appearance that may be shaped "rounded or oval" upon clinical observation.[4][14] The cyst is found to frequently reside at the anterior of the jaw.[2] Scans present a distribution of the cyst commonly at the upper jaw, where there is a 71.8% prevalence in cases.[2] The margin surrounding the cyst is usually occupied with a scalloped definition.[2] A bilateral presentation of the cyst is possible but is not common at the maxilla and mandible sites.[12] Analysis of scans allow physicians to differentiate the cyst and avoid misdiagnosis from other parallel lesions, i.e., ‘lateral periodontal cyst’ and ‘ameloblastoma’.[14] Scans can display the severity of cortical plate, root, and tooth impairment, which is analysed to determine the necessary action for reconstruction.[14] The cyst has an average size of 4.9 cm that can develop over the midline from the mandible or maxilla region.[13][3]
Histology
Histological features related to the cyst differ in each scenario; however, there is a general criterion to identify this entity.[13] The cyst can feature as a stratified squamous epithelium attached to fibrous connective tissue that is infiltrated by active immune cells.[2] The lining of the epithelium is occupied with a very small diameter and is usually non-keratinised.[7][12] Whereas, the lining of the lesion has an inconsistent length of diameter.[2] The basal cells is associated with no origin to a carcinoma.[11] Tissue cells may be faced with an abnormal increase in the concentration of calcium, which can cause the region to calcify.[5] The transformation of the epithelium is associated with a focal luminal development.[2] Eosinophilic organelles such as columnar and cuboidal cells can be observable during microscopy.[10] Intra-epithelial crypts may be apparent in the internal framework of the epithelium or at the external space where it presents itself as papillae protrusions.[7][12] Mucin is observable after the application of alcian blue dye on the tissue specimen.[7] The histological observation of goblet cells is also featured in the odontogenic dentigerous cyst.[10] In some circumstances, the epithelium can have variable plaque structures that appear as swirls in the tissue layers.[7] Interestingly, histologists were able to identify hyaline bodies within the tissue framework of the cyst.[5] It is encouraged that the histological identification of at least seven of these biological characteristics is required to accurately distinguish the cyst.[10]
Intraepithelial Hemosiderin
Pathologists have identified hemosiderin pigments that are unique to the glandular odontogenic cyst.[11] The discovery of this pigment can be pivotal to the differentiation of the cyst from other lesions.[11] The staining in the epithelium is due to the haemorrhaging at the lining.[11] The cause of the haemorrhaging can be triggered by the type of treatment, cellular degradation, or structural deformation induced by the cystic growth.[11] Examination of the cyst tissue section indicated that red blood cells from the intraluminal space was combined with extracellular constituents.[11] This process is carried out through transepithelial elimination.[11] This observational aspect is beneficial to determine the benign or malignant nature of the potential cancerous cyst.[11]
Immunocytochemistry
The examination of cytokeratin profiles is deemed useful when observing the differences between the glandular odontogenic cyst and central mucoepidermoid carcinoma.[13] These two lesions show individualised expression for cytokeratin 18 and 19.[5] The presence of osteodentin is supports the concept of an odontogenic pathway.[9] Past studies observed Ki-67, p53, and PCNA expression in common jaw cysts that share similar characteristics.[5] There is a lack of p53 expression found in radicular cysts.[5] Similarly, Ki-67 is seen less in the central mucoepidermoid carcinoma compared to the other lesions, though this discovery is not essential to the process of differential diagnosis.[5][13] Proliferating cell nuclear antigen readings are established to have no role in the differentiation process.[13] The TGF-beta marker is present in the cyst and can explain the limited concentration of normal functioning cells.[15]
MAML2 rearrangement
The observation of MAML2 rearrangement is described as a component useful in the differential diagnosis of the glandular odontogenic cyst and the closely related lesion, central mucoepidermoid carcinoma.[10] A second cystic development displayed the presence of CRTC3-MAML2 fusion after the in-vitro application.[10] The MAML2 rearrangement represents the developmental growth of central mucoepidermoid carcinoma from the glandular odontogenic cyst.[10] The use of fusion-gene transcript may be helpful towards the differentiation of the cyst from central mucoepidermoid carcinoma of the jaw and salivary glands.[10]
Treatment
Pre-treatment protocols

A computed tomography and panoramic x-ray must be undertaken in order to observe the severity of internal complications.[14] From these scans, physicians will observe the size, radiolucency, cortical bone, dentition, root, and vestibular zone.[14] In some cases, the dentition may be embedded into the cavity walls of the lesion, depending on the position of expansion at the odontogenic tissue.[12] The diagnosis of a smaller sized cyst is related to the attachment of only two teeth.[6] An expansive cyst develops over two teeth.[6] Presentation of a greater sized lesion requires a biopsy to determine the differential diagnosis for a precise treatment plan.[6]
Treatment process
The unilocular and multilocular nature is imperative to the determination of treatment style.[6] Local anesthesia is regularly provided as the cyst is embedded within the tissue structure of the jaw and requires an invasive procedure for a safe and precise extraction.[2] For unilocular cysts with minimal tissue deterioration, "enucleation, curettage, and marsupialization" are a suitable treatment plan.[6] Notably, the individual performance of enucleation or curettage as the primary action is linked to an incomplete extraction of the cyst and is only recommended to the less invasive lesions.[6] Multilocular cysts require a more invasive procedure "(i.e. peripheral ostectomy, marginal resection, or partial jaw resection)".[6] Cysts that are associated with more severe structural damage are endorsed to undergo marsupialization as either an initial or supplementary surgery.[6] The frequency of reappearance is likely associated with the lingering cystic tissue structures that remain after the performance of curettage.[12] The incorporation of a "dredging method (i.e. repetition of enucleation and curettage)" is also applied for those at a high-risk, until the remnants of the lesion diminishes for certain.[8] The treatment ensures scar tissue is removed to promote the proper reconstruction of osseous material for jaw preservation.[8] Alongside the main treatments, bone allograft application, cryosurgery, Carnoy's solution, and an apicoectomy are available but have not been consistently recommended.[12][14][8]The chloroform-free version of this fixative solution is recommended with the treatment type as it degenerates the remaining damaged dental lamina.[12] The most effective type of treatment remains unknown due to the lack of data from reported cases.[3]
Post-treatment protocols
Strict follow-up appointments are necessary after the removal of the cyst due to its high chances of remission, which is exacerbated in cases dealing with cortical plate perforation.[14][12] The glandular odontogenic cyst has a significant remission rate of 21 to 55% that can potentially develop during the period of 0.5 to 7 years post-surgery.[5][6] Cases occupied with a lower risk lesion are expected to follow-up with physicians for up to three years post-surgery, similar to the overlapping lesion odontogenic keratocyst.[14][6] A higher-risk situation is encouraged to consistently consult with physicians during a seven-year period after treatment.[12] Remission events need immediate attention with appropriate procedures such as enucleation or curettage.[6] In more harmful cases of remission, tissue resection, and marsupialization are carried out.[5]
Epidemiology
The clinical presentation of this cyst is very low in the population as noted by the 0.12 to 0.13% occurrence rate, extrapolated from a sample size of the 181 people.[2] The cyst mainly affects older individuals in the population, especially those that are in their 40 to 60s.[7] However, this cyst can impact younger individuals (i.e. 11), and more older individuals (i.e. 82) in the population.[2] The age distribution starts at a much lower number for people living in Asia and Africa.[2] Notably, those in their first 10 years of life have not been diagnosed with this cyst.[13] The cyst does present a tendency to proliferate in more males than females.[3] There is no definitive conclusion towards the relevance of gender and its influence on the rate of incidence.[5]
References
- ^ a b Borges, Leandro Bezerra; Fechine, Francisco Vagnaldo; Mota, Mário Rogério Lima; Sousa, Fabrício Bitu; Alves, Ana Paula Negreiros Nunes (March 2012). "Odontogenic lesions of the jaw: a clinical-pathological study of 461 cases". Revista Gaúcha de Odontologia. 60 (1): 71–78. S2CID 46982083.
- ^ a b c d e f g h i j k l m n o p Faisal, Mohammad; Ahmad, Syed Ansar; Ansari, Uzma (September 2015). "Glandular odontogenic cyst – Literature review and report of a paediatric case". Journal of Oral Biology and Craniofacial Research. 5 (3): 219–225. doi:10.1016/j.jobcr.2015.06.011. PMC 4623883. PMID 26587384.
- ^ a b c d e f g h Momeni Roochi, Mehrnoush; Tavakoli, Iman; Ghazi, Fatemeh Mojgan; Tavakoli, Ali (1 July 2015). "Case series and review of glandular odontogenic cyst with emphasis on treatment modalities". Journal of Cranio-Maxillofacial Surgery. 43 (6): 746–750. doi:10.1016/j.jcms.2015.03.030. PMID 25971944.
- ^ a b c d e f g h i Patel, Govind; Shah, Monali; Kale, Hemant; Ranginwala, Amena (2014). "Glandular odontogenic cyst: A rare entity". Journal of Oral and Maxillofacial Pathology. 18 (1): 89. doi:10.4103/0973-029X.131922. PMC 4065455. PMID 24959044.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i j k l m n o p q r Shear, Mervyn; Speight, Paul, eds. (2007). "Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst)". Cysts of the Oral and Maxillofacial Regions. pp. 94–99. doi:10.1002/9780470759769.ch7. ISBN 978-0-470-75976-9.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ a b c d e f g h i j k l m n o Kaplan, Ilana; Gal, Gavriel; Anavi, Yakir; Manor, Ronen; Calderon, Shlomo (April 2005). "Glandular odontogenic cyst: Treatment and recurrence". Journal of Oral and Maxillofacial Surgery. 63 (4): 435–441. doi:10.1016/j.joms.2004.08.007. PMID 15789313.
- ^ a b c d e f g h Prabhu, Sudeendra; Rekha, K; Kumar, GS (2010). "Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma". Journal of Oral and Maxillofacial Pathology. 14 (1): 12–5. doi:10.4103/0973-029X.64303. PMC 2996005. PMID 21180452.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e Motooka, Naomi; Ohba, Seigo; Uehara, Masataka; Fujita, Syuichi; Asahina, Izumi (1 January 2015). "A case of glandular odontogenic cyst in the mandible treated with the dredging method". Odontology. 103 (1): 112–115. doi:10.1007/s10266-013-0143-0. PMID 24374982. S2CID 21059170.
- ^ a b c d Shah, AmishaA; Sangle, Amit; Bussari, Smita; Koshy, AjitV (2016). "Glandular odontogenic cyst: A diagnostic dilemma". Indian Journal of Dentistry. 7 (1): 38–43. doi:10.4103/0975-962X.179371. PMC 4836096. PMID 27134453.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h Nagasaki, Atsuhiro; Ogawa, Ikuko; Sato, Yukiko; Takeuchi, Kengo; Kitagawa, Masae; Ando, Toshinori; Sakamoto, Shinnichi; Shrestha, Madhu; Uchisako, Kaori; Koizumi, Koichi; Toratani, Shigeaki; Konishi, Masaru; Takata, Takashi (January 2018). "Central mucoepidermoid carcinoma arising from glandular odontogenic cyst confirmed by analysis of MAML2 rearrangement: A case report: Central MEC arising from GOC". Pathology International. 68 (1): 31–35. doi:10.1111/pin.12609. PMID 29131467. S2CID 8932602.
- ^ a b c d e f g h i j k AbdullGaffar, Badr; Koilelat, Mohamed (May 2017). "Glandular Odontogenic Cyst: The Value of Intraepithelial Hemosiderin". International Journal of Surgical Pathology. 25 (3): 250–252. doi:10.1177/1066896916672333. PMID 27829208. S2CID 46588216.
- ^ a b c d e f g h i j k l m Akkaş, İsmail; Toptaş, Orçun; Özan, Fatih; Yılmaz, Fahri (1 March 2015). "Bilateral Glandular Odontogenic Cyst of Mandible: A Rare Occurrence". Journal of Maxillofacial and Oral Surgery. 14 (1): 443–447. doi:10.1007/s12663-014-0668-y. PMC 4379287. PMID 25848155.
- ^ a b c d e f g h i j Neville, Brad W. (2016). "Cyst, Glandular Odontogenic". Encyclopedia of Soil Science. Encyclopedia of Earth Sciences Series. pp. 89–93. doi:10.1007/978-3-319-28085-1_677. ISBN 978-1-4020-3994-2.
- ^ a b c d e f g h i j Cano, Jorge; Benito, Dulce María; Montáns, José; Rodríguez-Vázquez, José Francisco; Campo, Julián; Colmenero, César (1 July 2012). "Glandular odontogenic cyst: Two high-risk cases treated with conservative approaches". Journal of Cranio-Maxillofacial Surgery. 40 (5): e131–e136. doi:10.1016/j.jcms.2011.07.005. PMID 21865053.
- ^ a b c d Alaeddini, Mojgan; Eshghyar, Nosratollah; Etemad‐Moghadam, Shahroo (2017). "Expression of podoplanin and TGF-beta in glandular odontogenic cyst and its comparison with developmental and inflammatory odontogenic cystic lesions". Journal of Oral Pathology & Medicine. 46 (1): 76–80. doi:10.1111/jop.12475. PMID 27391558. S2CID 40879254.
Bibliography
- AbdullGaffar, Badr; Koilelat, Mohamed (May 2017). "Glandular Odontogenic Cyst: The Value of Intraepithelial Hemosiderin". International Journal of Surgical Pathology. 25 (3): 250–252. doi:10.1177/1066896916672333. PMID 27829208. S2CID 46588216.
- Akkaş, İsmail; Toptaş, Orçun; Özan, Fatih; Yılmaz, Fahri (1 March 2015). "Bilateral Glandular Odontogenic Cyst of Mandible: A Rare Occurrence". Journal of Maxillofacial and Oral Surgery. 14 (1): 443–447. doi:10.1007/s12663-014-0668-y. PMC 4379287. PMID 25848155.
- Alaeddini, Mojgan; Eshghyar, Nosratollah; Etemad‐Moghadam, Shahroo (2017). "Expression of podoplanin and TGF-beta in glandular odontogenic cyst and its comparison with developmental and inflammatory odontogenic cystic lesions". Journal of Oral Pathology & Medicine. 46 (1): 76–80. doi:10.1111/jop.12475. PMID 27391558. S2CID 40879254.
- Borges, Leandro Bezerra; Fechine, Francisco Vagnaldo; Mota, Mário Rogério Lima; Sousa, Fabrício Bitu; Alves, Ana Paula Negreiros Nunes (March 2012). "Odontogenic lesions of the jaw: a clinical-pathological study of 461 cases". Revista Gaúcha de Odontologia. 60 (1): 71–78. S2CID 46982083.
- Cano, Jorge; Benito, Dulce María; Montáns, José; Rodríguez-Vázquez, José Francisco; Campo, Julián; Colmenero, César (1 July 2012). "Glandular odontogenic cyst: Two high-risk cases treated with conservative approaches". Journal of Cranio-Maxillofacial Surgery. 40 (5): e131–e136. doi:10.1016/j.jcms.2011.07.005. PMID 21865053.
- Faisal, Mohammad; Ahmad, Syed Ansar; Ansari, Uzma (September 2015). "Glandular odontogenic cyst – Literature review and report of a paediatric case". Journal of Oral Biology and Craniofacial Research. 5 (3): 219–225. doi:10.1016/j.jobcr.2015.06.011. PMC 4623883. PMID 26587384.
- Kaplan, Ilana; Gal, Gavriel; Anavi, Yakir; Manor, Ronen; Calderon, Shlomo (April 2005). "Glandular odontogenic cyst: Treatment and recurrence". Journal of Oral and Maxillofacial Surgery. 63 (4): 435–441. doi:10.1016/j.joms.2004.08.007. PMID 15789313.
- Motooka, Naomi; Ohba, Seigo; Uehara, Masataka; Fujita, Syuichi; Asahina, Izumi (1 January 2015). "A case of glandular odontogenic cyst in the mandible treated with the dredging method". Odontology. 103 (1): 112–115. doi:10.1007/s10266-013-0143-0. PMID 24374982. S2CID 21059170.
- Nagasaki, Atsuhiro; Ogawa, Ikuko; Sato, Yukiko; Takeuchi, Kengo; Kitagawa, Masae; Ando, Toshinori; Sakamoto, Shinnichi; Shrestha, Madhu; Uchisako, Kaori; Koizumi, Koichi; Toratani, Shigeaki; Konishi, Masaru; Takata, Takashi (January 2018). "Central mucoepidermoid carcinoma arising from glandular odontogenic cyst confirmed by analysis of MAML2 rearrangement: A case report: Central MEC arising from GOC". Pathology International. 68 (1): 31–35. doi:10.1111/pin.12609. PMID 29131467. S2CID 8932602.
- Neville, Brad W. (2016). "Cyst, Glandular Odontogenic". Encyclopedia of Soil Science. Encyclopedia of Earth Sciences Series. pp. 89–93. doi:10.1007/978-3-319-28085-1_677. ISBN 978-1-4020-3994-2.
- Prabhu, Sudeendra; Rekha, K; Kumar, GS (2010). "Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma". Journal of Oral and Maxillofacial Pathology. 14 (1): 12–5. doi:10.4103/0973-029X.64303. PMC 2996005. PMID 21180452.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Momeni Roochi, Mehrnoush; Tavakoli, Iman; Ghazi, Fatemeh Mojgan; Tavakoli, Ali (1 July 2015). "Case series and review of glandular odontogenic cyst with emphasis on treatment modalities". Journal of Cranio-Maxillofacial Surgery. 43 (6): 746–750. doi:10.1016/j.jcms.2015.03.030. PMID 25971944.
- Patel, Govind; Shah, Monali; Kale, Hemant; Ranginwala, Amena (2014). "Glandular odontogenic cyst: A rare entity". Journal of Oral and Maxillofacial Pathology. 18 (1): 89. doi:10.4103/0973-029X.131922. PMC 4065455. PMID 24959044.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Shah, AmishaA; Sangle, Amit; Bussari, Smita; Koshy, AjitV (2016). "Glandular odontogenic cyst: A diagnostic dilemma". Indian Journal of Dentistry. 7 (1): 38–43. doi:10.4103/0975-962X.179371. PMC 4836096. PMID 27134453.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Shear, Mervyn; Speight, Paul, eds. (2007). "Glandular Odontogenic Cyst (Sialo-Odontogenic Cyst)". Cysts of the Oral and Maxillofacial Regions. pp. 94–99. doi:10.1002/9780470759769.ch7. ISBN 978-0-470-75976-9.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)
Further reading
- Kahn MA (2001). Basic Oral and Maxillofacial Pathology. Vol. 1.
