Zidovudine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Retrovir, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a687007 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous, rectal suppository |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Complete absorption, following first-pass metabolism systemic availability 75% (range 52 to 75%) |
| Protein binding | 30 to 38% |
| Metabolism | Liver |
| Elimination half-life | 0.5 to 3 hours |
| Excretion | Kidney and Bile duct |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.152.492 |
| Chemical and physical data | |
| Formula | C10H13N5O4 |
| Molar mass | 267.245 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Zidovudine (ZDV), also known as azidothymidine (AZT), was the first antiretroviral medication used to prevent and treat HIV/AIDS. It is generally recommended for use in combination with other antiretrovirals.[6] It may be used to prevent mother-to-child spread during birth or after a needlestick injury or other potential exposure.[6] It is sold both by itself and together as lamivudine/zidovudine and abacavir/lamivudine/zidovudine.[6] It can be used by mouth or by slow injection into a vein.[6]
Common side effects include headaches, fever, and nausea.[6] Serious side effects include liver problems, muscle damage, and high blood lactate levels.[6] It is commonly used in pregnancy and appears to be safe for the fetus.[6] ZDV is of the nucleoside analog reverse-transcriptase inhibitor (NRTI) class.[6] It works by inhibiting the enzyme reverse transcriptase that HIV uses to make DNA and therefore decreases replication of the virus.[6]
Zidovudine was first described in 1964.[7] It was resynthesized from a public-domain formula by Burroughs Wellcome.[8] It was approved in the United States in 1987 and was the first treatment for HIV.[6][9] It is on the World Health Organization's List of Essential Medicines.[10][11] It is available as a generic medication.[6]
Medical uses
[edit]HIV treatment
[edit]AZT was usually dosed twice a day in combination with other antiretroviral therapies. This approach is referred to as Highly Active Antiretroviral Therapy (HAART) and is used to prevent the likelihood of HIV resistance.[12][13] As of 2019, the standard is a three-drug once-daily oral treatment that can include AZT.[14]
HIV prevention
[edit]AZT has been used for post-exposure prophylaxis (PEP) in combination with another antiretroviral drug called lamivudine. Together they work to substantially reduce the risk of HIV infection following the first single exposure to the virus.[15] More recently, AZT has been replaced by other antiretrovirals such as tenofovir to provide PEP.[16] Before tenofovir, a principal part of the clinical pathway for both pre-exposure prophylaxis and post-exposure treatment of mother-to-child transmission of HIV during pregnancy, labor, and delivery and has been proven to be integral to uninfected siblings' perinatal and neonatal development.[17][18] Without AZT, 10–15% of fetuses with HIV-infected mothers will themselves become infected.[19] AZT has been shown to reduce this risk to 8% when given in a three-part regimen post-conception, delivery, and six weeks post-delivery. Consistent and proactive precautionary measures, such as the rigorous use of antiretroviral medications, cesarean section, face masks, heavy-duty rubber gloves, clinically segregated disposable diapers, and avoidance of mouth contact will further reduce child-attendant transmission of HIV to as little as 1–2%.[20][21][22]
During 1994 to 1999, AZT was the primary form of prevention of mother-to-child HIV transmission. AZT prophylaxis prevented more than 1000 parental and infant deaths from AIDS in the United States.[23] In the U.S. at that time, the accepted standard of care for HIV-positive mothers was known as the 076 regimen and involved five daily doses of AZT from the second trimester onwards, as well as AZT intravenously administered during labour.[24] As this treatment was lengthy and expensive, it was deemed unfeasible in the Global South, where mother-to-child transmission was a significant problem. A number of studies were initiated in the late 1990s that sought to test the efficacy of a shorter, simpler regimen for use in 'resource-poor' countries.[25] This AZT short course was an inferior standard of care and would have been considered malpractice if trialed in the US; however, it was nonetheless a treatment that would improve the care and survival of impoverished subjects.[25]
Antibacterial properties
[edit]Zidovudine also has antibacterial properties,[26] though not routinely used in clinical settings. It acts on bacteria with a mechanism of action still not fully explained. Promising results from in vitro and in vivo studies showed the efficacy of AZT also against multidrug-resistant gram-negative bacteria (including mcr-1 carrying and metallo-β-lactamase producing isolates), especially in combination with other active agents (e.g. fosfomycin, colistin, tigecycline).[27][28]
Side effects
[edit]Most common side effects include nausea, vomiting, acid reflux (heartburn), headache, cosmetic reduction in abdominal body fat, trouble sleeping, and loss of appetite. Less common side effects include faint discoloration of fingernails and toenails, mood elevation, occasional tingling or transient numbness of the hands or feet, and minor skin discoloration. Allergic reactions are rare.[29]
Early long-term higher-dose therapy with AZT was initially associated with side effects that sometimes limited therapy, including anemia, neutropenia, hepatotoxicity, cardiomyopathy, and myopathy. All of these conditions were generally found to be reversible upon reduction of AZT dosages. They have been attributed to several possible causes, including transient depletion of mitochondrial DNA, sensitivity of the γ-DNA polymerase in some cell mitochondria,[30] the depletion of thymidine triphosphate, oxidative stress, reduction of intracellular L-carnitine or apoptosis of the muscle cells.[31] Anemia due to AZT was successfully treated using erythropoetin to stimulate red blood cell production.[32][33] Drugs that inhibit hepatic glucuronidation, such as indomethacin, nordazepam, acetylsalicylic acid (aspirin) and trimethoprim decreased the elimination rate and increased the therapeutic strength of the medication.[34] Today, side effects are much less common with the use of lower doses of AZT.[35] According to IARC, there is sufficient evidence in experimental animals for the carcinogenicity of zidovudine; it is possibly carcinogenic to humans (Group 2B).[36] In 2009, the State of California added zidovudine to its list of chemicals "known to the state of California to cause cancer and other reproductive harm."[37]
Viral resistance
[edit]Even at the highest doses that can be tolerated in patients, AZT is not potent enough to prevent all HIV replication and may only slow the replication of the virus and progression of the disease. Prolonged AZT treatment can lead to HIV developing resistance to AZT by mutation of its reverse transcriptase.[38][39] To slow the development of resistance, physicians generally recommend that AZT be given in combination with another reverse-transcriptase inhibitor and an antiretroviral from another group, such as a protease inhibitor, non-nucleoside reverse-transcriptase inhibitor, or integrase inhibitor; this type of therapy is known as HAART (Highly Active Anti Retroviral Therapy).
Mechanism of action
[edit]
AZT is a thymidine analogue. AZT works by selectively inhibiting HIV's reverse transcriptase, the enzyme that the virus uses to make a DNA copy of its RNA. Reverse transcription is necessary for production of HIV's double-stranded DNA, which would be subsequently integrated into the genetic material of the infected cell (where it is called a provirus).[40][41][42]
Cellular enzymes convert AZT into the effective 5'-triphosphate form. Studies have shown that the termination of HIV's forming DNA chains is the specific factor in the inhibitory effect.[43]
At very high doses, AZT's triphosphate form may also inhibit DNA polymerase used by human cells to undergo cell division, but regardless of dosage AZT has an approximately 100-fold greater affinity for HIV's reverse transcriptase.[44] The selectivity has been suggested to be due to the cell's ability to quickly repair its own DNA chain if it is disrupted by AZT during its formation, whereas the HIV virus lacks that ability.[45] Thus AZT inhibits HIV replication without affecting the function of uninfected cells.[40] At sufficiently high dosages, AZT begins to inhibit the cellular DNA polymerase used by mitochondria to replicate, accounting for its potentially toxic but reversible effects on cardiac and skeletal muscles, causing myositis.[46][47][48][49][50]
Chemistry
[edit]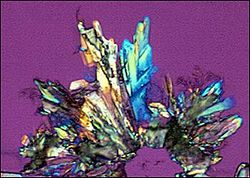
Enantiopure AZT crystallizes in the monoclinic space group P21. The primary intermolecular bonding motif is a hydrogen bonded dimeric ring formed from two N-H...O interactions.[51][52]
History
[edit]Initial cancer research
[edit]In the 1960s, the theory that most cancers were caused by environmental retroviruses gained clinical support and funding. It had recently become known, due to the work of Nobel laureates Howard Temin and David Baltimore,[53] that nearly all avian cancers were caused by bird retroviruses, but corresponding human retroviruses had not yet been found.
In parallel work, other compounds that successfully blocked the synthesis of nucleic acids had been proven to be both antibacterial, antiviral, and anticancer agents, the leading work being done at the laboratory of Nobel laureates George H. Hitchings and Gertrude Elion, leading to the development of the antitumor agent 6-mercaptopurine.[54]
Richard E. Beltz first synthesized AZT in 1961, but did not publish his research.[55][56]Jerome Horwitz of the Barbara Ann Karmanos Cancer Institute and Wayne State University School of Medicine synthesized AZT in 1964 under a US National Institutes of Health (NIH) grant.[57][58][59] Development was shelved after it proved biologically inert in mice.[57][60] In 1974, Wolfram Ostertag of the Max Planck Institute for Experimental Medicine in Göttingen, Germany, reported that AZT specifically targeted Friend virus (strain of murine leukemia virus).[61]
This report attracted little interest from other researchers as the Friend leukemia virus is a retrovirus, and at the time, there were no known human diseases caused by retroviruses.[62]
HIV/AIDS research
[edit]In 1983, researchers at the Institut Pasteur in Paris identified the retrovirus now known as the Human Immunodeficiency Virus (HIV) as the cause of acquired immunodeficiency syndrome (AIDS) in humans.[63][64] Shortly thereafter, Samuel Broder, Hiroaki Mitsuya, and Robert Yarchoan of the United States National Cancer Institute (NCI) initiated a program to develop therapies for HIV/AIDS.[65] Using a line of CD4+ T cells that they had made, they developed an assay to screen drugs for their ability to protect CD4+ T cells from being killed by HIV. In order to expedite the process of discovering a drug, the NCI researchers actively sought collaborations with pharmaceutical companies having access to libraries of compounds with potential antiviral activity.[40] This assay could simultaneously test both the anti-HIV effect of the compounds and their toxicity against infected T cells.
In June 1984, Burroughs-Wellcome virologist Marty St. Clair set up a program to discover drugs with the potential to inhibit HIV replication. Burroughs-Wellcome had expertise in nucleoside analogs and viral diseases, led by researchers including George Hitchings, Gertrude Elion, David Barry, Paul (Chip) McGuirt Jr., Philip Furman, Martha St. Clair, Janet Rideout, Sandra Lehrman and others. Their research efforts were focused in part on the viral enzyme reverse transcriptase. Reverse transcriptase is an enzyme that retroviruses, including HIV, utilize to replicate themselves. Secondary testing was performed in mouse cells infected with the retroviruses Friend virus or Harvey sarcoma virus, as the Wellcome group did not have a viable in-house HIV antiviral assay in place at that time, and these other retroviruses were believed to represent reasonable surrogates. AZT proved to be a remarkably potent inhibitor of both Friend virus and Harvey sarcoma virus, and a search of the company's records showed that it had demonstrated low toxicity when tested for its antibacterial activity in rats many years earlier. Based in part on these results, AZT was selected by nucleoside chemist Janet Rideout as one of 11 compounds to send to the NCI for testing in that organization's HIV antiviral assay.[62]
In February 1985, the NCI scientists found that AZT had potent efficacy in vitro.[40][57] Several months later, a phase 1 clinical trial of AZT at the NCI was initiated at the NCI and Duke University.[41][46][66] In doing this Phase I trial, they built on their experience in doing an earlier trial, with suramin, another drug that had shown effective anti-HIV activity in the laboratory. This initial trial of AZT proved that the drug could be safely administered to patients with HIV, that it increased their CD4 counts, restored T cell immunity as measured by skin testing, and that it showed strong evidence of clinical effectiveness, such as inducing weight gain in AIDS patients. It also showed that levels of AZT that worked in vitro could be injected into patients in serum and suppository form, and that the drug penetrated deeply only into infected brains.
Patent filed and FDA approval
[edit]A flawed double-blind, placebo-controlled randomized trial of AZT was subsequently conducted by Burroughs-Wellcome and suggested that AZT safely prolongs the lives of people with HIV. However, it was quickly unblinded and several more in the drug receiving group later perished.[67][68] Burroughs-Wellcome filed for a patent for AZT in 1985. The Anti-Infective Advisory Committee to United States Food and Drug Administration (FDA) voted ten to one to recommend the approval of AZT.[69] The FDA approved the drug (via the then-new FDA accelerated approval system) for use against HIV, AIDS, and AIDS Related Complex (ARC, a now-obsolete medical term for pre-AIDS illness) on March 20, 1987.[70] The time between the first demonstration that AZT was active against HIV in the laboratory and its approval was 25 months.
AZT was subsequently approved unanimously for infants and children in 1990.[71] AZT was initially administered in significantly higher dosages than today, typically 400 mg every four hours, day and night, compared to modern dosage of 300 mg twice daily.[72] The paucity of alternatives for treating HIV/AIDS at that time unambiguously affirmed the health risk/benefit ratio, with inevitable slow, disfiguring, and painful death from HIV outweighing the drug's side effect of transient anemia and malaise.
Society and culture
[edit]Until 1991, 80% of the $420 million allocated to the National Institute of Health's AIDS Clinical Trials Group, went toward studies of AZT. Aside from two similarly designed chemotherapies, ddI and ddC, from approval of the drug until 1993, no other drugs against AIDS were approved, leading to criticism that research preoccupation with AZT and its close relatives, and the massive diverting of funds to such, had delayed the development of more efficacious drugs.[8]
In 1991, the advocacy group Public Citizen filed a lawsuit claiming that the patents were invalid. Subsequently, Barr Laboratories and Novopharm Ltd. also challenged the patent, in part based on the assertion that NCI scientists Samuel Broder, Hiroaki Mitsuya, and Robert Yarchoan should have been named as inventors, and those two companies applied to the FDA to sell AZT as a generic drug. In response, Burroughs Wellcome Co. filed a lawsuit against the two companies. The United States Court of Appeals for the Federal Circuit ruled in 1992 in favor of Burroughs Wellcome, ruling that even though they had never tested it against HIV, they had conceived of it working before they sent it to the NCI scientists. This suit was appealed up to the Supreme Court of the US, but in 1996 the Court declined to formally review it.[73] The case, Burroughs Wellcome Co. v. Barr Laboratories, was a landmark in US law of inventorship.[74]
In 2002, another lawsuit was filed challenging the patent by the AIDS Healthcare Foundation, which also filed an antitrust case against GSK.[75] The patent case was dismissed in 2003 and AHF filed a new case challenging the patent.[75]
GSK's patents on AZT expired in 2005, and in September 2005, the FDA approved three generic versions.[76]
References
[edit]- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved October 22, 2023.
- ^ "Retrovir 100mg Capsules – Summary of Product Characteristics (SmPC)". (emc). December 14, 2018. Retrieved January 23, 2021.
- ^ "Retrovir – zidovudine capsule Retrovir – zidovudine solution Retrovir – zidovudine injection, solution". DailyMed. Retrieved January 23, 2021.
- ^ "Active substance: Zidovudine" (PDF). European Medicines Agency. November 30, 2017.
- ^ "Zidovudine". PubChem Public Chemical Database. NCBI. Archived from the original on October 25, 2012. Retrieved April 10, 2011.
- ^ a b c d e f g h i j k "Zidovudine". The American Society of Health-System Pharmacists. Archived from the original on December 21, 2016. Retrieved November 28, 2016.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 505. ISBN 9783527607495. Archived from the original on September 8, 2017.
- ^ a b Linda Marsa, 'Toxic Hope', Los Angeles Times, 20 June 1993
- ^ Reeves JD, Derdeyn CA (2007). Entry Inhibitors in HIV Therapy. Springer Science & Business Media. p. 179. ISBN 9783764377830.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list. Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ De Clercq E (January 1994). "HIV resistance to reverse transcriptase inhibitors". Biochemical Pharmacology. 47 (2): 155–169. doi:10.1016/0006-2952(94)90001-9. PMID 7508227.
- ^ Yarchoan R, Mitsuya H, Broder S (October 1988). "AIDS therapies". Scientific American. 259 (4): 110–119. Bibcode:1988SciAm.259d.110Y. doi:10.1038/scientificamerican1088-110. PMID 3072667.
- ^ Phanuphak N, Gulick RM (January 2020). "HIV treatment and prevention 2019: current standards of care". Current Opinion in HIV and AIDS. 15 (1): 4–12. doi:10.1097/COH.0000000000000588. PMID 31658110. S2CID 204952772.
- ^ Panlilio AL, Cardo DM, Grohskopf LA, Heneine W, Ross CS (September 2005). "Updated U.S. Public Health Service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis" (PDF). MMWR Recomm Rep. 54 (RR-9): 1–17. PMID 16195697.
- ^ "UK guideline for the use of post-exposure prophylaxis for HIV following sexual exposure (2011)". Archived from the original on April 8, 2014. Retrieved April 7, 2014.
- ^ "Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health" (PDF). AIDSinfo. U.S. Department of Health and Human Services. November 17, 2005. Archived from the original (PDF) on April 22, 2006. Retrieved March 29, 2006.
- ^ Briand N, Lallemant M, Jourdain G, Techapalokul S, Tunthanathip P, Suphanich S, et al. (April 2007). "Haematological safety of perinatal zidovudine in pregnant HIV-1-infected women in Thailand: secondary analysis of a randomized trial". PLOS Clinical Trials. 2 (4): e11. doi:10.1371/journal.pctr.0020011. PMC 1863515. PMID 17476315.
- ^ Science Codex.
- ^ CIDRZ. Prevention of AIDS Transmission (PMTCT). "Prevention of mother-to-child HIV transmission (PMTCT) | CIDRZ". Archived from the original on February 14, 2012. Retrieved March 31, 2012.
- ^ Transmission of HIV from infants "Transmission of HIV from infants to women who breastfeed them". Aids Perspective. July 1, 2012. Archived from the original on December 3, 2013. Retrieved August 3, 2012.
- ^ Connor E, Sperling R, Gelber R, Kiselev P, Scott G, O'Sullivan M, VanDyke R, Bey M, Shearer W, Jacobson R (1994). "Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group". N Engl J Med. 331 (18): 1173–80. doi:10.1056/NEJM199411033311801. PMID 7935654. S2CID 13457499.
- ^ Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. (July 2006). "The survival benefits of AIDS treatment in the United States". The Journal of Infectious Diseases. 194 (1): 11–19. doi:10.1086/505147. PMID 16741877.
- ^ Morris K (February 1998). "Short course of AZT halves HIV-1 perinatal transmission". Lancet. 351 (9103): 651. doi:10.1016/S0140-6736(05)78436-1. PMID 9500334. S2CID 8293828.
- ^ a b Crane J (December 2010). "Adverse events and placebo effects: African scientists, HIV, and ethics in the 'global health sciences'". Social Studies of Science. 40 (6): 843–870. doi:10.1177/0306312710371145. PMID 21553555. S2CID 26027925.
- ^ DeSarno AE, Parcell BJ, Coote PJ (December 2020). "Repurposing the anti-viral drug zidovudine (AZT) in combination with meropenem as an effective treatment for infections with multi-drug resistant, carbapenemase-producing strains of Klebsiella pneumoniae". Pathogens and Disease. 78 (9): ftaa063. doi:10.1093/femspd/ftaa063. hdl:10023/24137. PMID 33053176.
- ^ Zhou YF, Liu P, Dai SH, Sun J, Liu YH, Liao XP (December 2020). "Activity of Tigecycline or Colistin in Combination with Zidovudine against Escherichia coli Harboring tet(X) and mcr-1". Antimicrobial Agents and Chemotherapy. 65 (1). doi:10.1128/AAC.01172-20. PMC 7927862. PMID 33020156.
- ^ Antonello RM, Di Bella S, Betts J, La Ragione R, Bressan R, Principe L, et al. (July 2021). "Zidovudine in synergistic combination with fosfomycin: an in vitro and in vivo evaluation against multidrug-resistant Enterobacterales". International Journal of Antimicrobial Agents. 58 (1): 106362. doi:10.1016/j.ijantimicag.2021.106362. PMID 34010710. S2CID 234791392.
- ^ "zidovudine, Retrovir". Medicinenet.com. August 12, 2010. Archived from the original on December 20, 2010. Retrieved December 14, 2010.
- ^ Sun R, Eriksson S, Wang L (June 2010). "Identification and characterization of mitochondrial factors modulating thymidine kinase 2 activity". Nucleosides, Nucleotides & Nucleic Acids. 29 (4–6): 382–385. doi:10.1080/15257771003741018. PMID 20544523. S2CID 13539181.
- ^ Scruggs ER, Dirks Naylor AJ (2008). "Mechanisms of zidovudine-induced mitochondrial toxicity and myopathy". Pharmacology. 82 (2): 83–88. doi:10.1159/000134943. PMID 18504416. S2CID 2044833.
- ^ Fisher JW (December 1997). "Erythropoietin: physiologic and pharmacologic aspects". Proceedings of the Society for Experimental Biology and Medicine. 216 (3): 358–369. doi:10.3181/00379727-216-44183. PMID 9402140. S2CID 26177904.
- ^ Fisher JW (January 2003). "Erythropoietin: physiology and pharmacology update". Experimental Biology and Medicine. 228 (1): 1–14. doi:10.1177/153537020322800101. PMID 12524467. S2CID 2829677.
- ^ "ZIDOVUDINE (AZT) – ORAL (Retrovir) side effects, medical uses, and drug interactions". MedicineNet. Archived from the original on June 30, 2005. Retrieved January 9, 2006.
- ^ Side Effects. NAM Aidsmap. "Zidovudine (AZT, Retrovir)". Archived from the original on December 26, 2011. Retrieved March 28, 2012.
- ^ "Summary of Data Reported and Evaluation". 2000. Archived from the original on January 4, 2012. Retrieved August 11, 2012.
- ^ "State of California Environmental Protection Agency Office of Environmental Hazard Assessment Safe Drinking Water and Toxic Enforcement Act of 1986 Chemicals Known to the State to Cause Cancer or Reproductive Toxicity July 29, 1011" (PDF). July 29, 2011. Retrieved November 14, 2022.
- ^ Richman DD (May 1990). "Susceptibility to nucleoside analogues of zidovudine-resistant isolates of human immunodeficiency virus". The American Journal of Medicine. 88 (5B): 8S–10S. doi:10.1016/0002-9343(90)90414-9. PMID 2186629.
- ^ Wainberg MA, Brenner BG, Turner D (May 2005). "Changing patterns in the selection of viral mutations among patients receiving nucleoside and nucleotide drug combinations directed against human immunodeficiency virus type 1 reverse transcriptase". Antimicrobial Agents and Chemotherapy. 49 (5): 1671–1678. doi:10.1128/AAC.49.5.1671-1678.2005. PMC 1087622. PMID 15855480.
- ^ a b c d Mitsuya H, Weinhold KJ, Furman PA, St Clair MH, Lehrman SN, Gallo RC, et al. (October 1985). "3'-Azido-3'-deoxythymidine (BW A509U): an antiviral agent that inhibits the infectivity and cytopathic effect of human T-lymphotropic virus type III/lymphadenopathy-associated virus in vitro". Proceedings of the National Academy of Sciences of the United States of America. 82 (20): 7096–7100. Bibcode:1985PNAS...82.7096M. doi:10.1073/pnas.82.20.7096. PMC 391317. PMID 2413459.
- ^ a b Yarchoan R, Klecker R, Weinhold K, Markham P, Lyerly H, Durack D, Gelmann E, Lehrman S, Blum R, Barry D (1986). "Administration of 3'-azido-3'-deoxythymidine, an inhibitor of HTLV-III/LAV replication, to patients with AIDS or AIDS-related complex". Lancet. 1 (8481): 575–80. doi:10.1016/S0140-6736(86)92808-4. PMID 2869302. S2CID 37985276.
- ^ Mitsuya H, Yarchoan R, Broder S (1990). "Molecular targets for AIDS therapy". Science (Submitted manuscript). 249 (4976): 1533–44. Bibcode:1990Sci...249.1533M. doi:10.1126/science.1699273. PMID 1699273.
- ^ Quan Y, Rong L, Liang C, Wainberg MA (August 1999). "Reverse transcriptase inhibitors can selectively block the synthesis of differently sized viral DNA transcripts in cells acutely infected with human immunodeficiency virus type 1". Journal of Virology. 73 (8): 6700–6707. doi:10.1128/JVI.73.8.6700-6707.1999. PMC 112754. PMID 10400767.
- ^ Furman PA, Fyfe JA, St Clair MH, Weinhold K, Rideout JL, Freeman GA, et al. (November 1986). "Phosphorylation of 3'-azido-3'-deoxythymidine and selective interaction of the 5'-triphosphate with human immunodeficiency virus reverse transcriptase". Proceedings of the National Academy of Sciences of the United States of America. 83 (21): 8333–8337. Bibcode:1986PNAS...83.8333F. doi:10.1073/pnas.83.21.8333. PMC 386922. PMID 2430286.
- ^ Induction of Endogenous Virus and of Thymidline Kinase. "Induction of Endogenous Virus and of Thymidline Kinase by Bromodeoxyuridine in Cell Cultures Transformed by Friend Virus" (PDF). Archived (PDF) from the original on September 24, 2015. Retrieved November 14, 2022.
- ^ a b Yarchoan R, Mitsuya H, Myers C, Broder S (1989). "Clinical pharmacology of 3'-azido-2',3'-dideoxythymidine (zidovudine) and related dideoxynucleosides". N Engl J Med. 321 (11): 726–38. doi:10.1056/NEJM198909143211106. PMID 2671731.
- ^ Collins ML, Sondel N, Cesar D, Hellerstein MK (September 2004). "Effect of nucleoside reverse transcriptase inhibitors on mitochondrial DNA synthesis in rats and humans". Journal of Acquired Immune Deficiency Syndromes. 37 (1): 1132–1139. doi:10.1097/01.qai.0000131585.77530.64. PMID 15319672. S2CID 20020419.
- ^ Parker WB, White EL, Shaddix SC, Ross LJ, Buckheit RW, Germany JM, et al. (January 1991). "Mechanism of inhibition of human immunodeficiency virus type 1 reverse transcriptase and human DNA polymerases alpha, beta, and gamma by the 5'-triphosphates of carbovir, 3'-azido-3'-deoxythymidine, 2',3'-dideoxyguanosine and 3'-deoxythymidine. A novel RNA template for the evaluation of antiretroviral drugs". The Journal of Biological Chemistry. 266 (3): 1754–1762. doi:10.1016/S0021-9258(18)52360-7. PMID 1703154.
- ^ Rang HP, Dale MM, Ritter JM (1995). Pharmacology (3rd ed.). Pearson Professional Ltd. ISBN 978-0-443-05974-2.
- ^ Balzarini J, Naesens L, Aquaro S, Knispel T, Perno C, De Clercq E, Meier C (December 1999). "Intracellular metabolism of CycloSaligenyl 3'-azido-2', 3'-dideoxythymidine monophosphate, a prodrug of 3'-azido-2', 3'-dideoxythymidine (zidovudine)". Molecular Pharmacology. 56 (6): 1354–1361. doi:10.1124/mol.56.6.1354. PMID 10570065. S2CID 25678740. Archived from the original on September 21, 2007.
- ^ Dyer I, Low JN, Tollin P, Wilson HR, Howie RA (April 1988). "Structure of 3'-azido-3'-deoxythymidine, AZT". Acta Crystallogr C. 44 (4): 767–9. Bibcode:1988AcCrC..44..767D. doi:10.1107/S0108270188000368. PMID 3271074.
- ^ Camerman A, Mastropaolo D, Camerman N (1987). "Azidothymidine: crystal structure and possible functional role of the azido group". Proc Natl Acad Sci USA. 84 (23): 8239–8242. Bibcode:1987PNAS...84.8239C. doi:10.1073/pnas.84.23.8239. PMC 299517. PMID 2446321.
- ^ "The Nobel Prize in Physiology or Medicine 1975". NobelPrize.org. Archived from the original on January 3, 2017.
- ^ "The Purine Path To Chemotherapy" (PDF). Archived from the original (PDF) on August 8, 2017.
- ^ Marsa L (June 20, 1993). "Toxic Hope: Widely Embraced, the AIDS Drug is now under Heavy Fire". Los Angeles Times.
- ^ Brinck A. "Inventing AZT" (PDF).
- ^ a b c Broder S (January 2010). "The development of antiretroviral therapy and its impact on the HIV-1/AIDS pandemic". Antiviral Research. 85 (1): 1–18. doi:10.1016/j.antiviral.2009.10.002. PMC 2815149. PMID 20018391.
- ^ Horwitz JP, Chua J, Noel MJ (1964). "The monomesylates of 1-(2-deoxy-bd-lyxofuranosyl) thymines". Org. Chem. Ser. Monogr. 29 (7): 2076–9. doi:10.1021/jo01030a546.
- ^ Detours V; Henry D (writers/directors) (2002). I am alive today (history of an AIDS drug) (Film). ADR Productions/Good & Bad News.
- ^ "A Failure Led to Drug Against AIDS". The New York Times. September 20, 1986. Archived from the original on August 16, 2009. Retrieved June 30, 2010.
- ^ Ostertag W, Roesler G, Krieg CJ, Kind J, Cole T, Crozier T, et al. (December 1974). "Induction of endogenous virus and of thymidine kinase by bromodeoxyuridine in cell cultures transformed by Friend virus". Proceedings of the National Academy of Sciences of the United States of America. 71 (12): 4980–4985. Bibcode:1974PNAS...71.4980O. doi:10.1073/pnas.71.12.4980. PMC 434023. PMID 4531031.
- ^ a b Sneader W (2006). Drug Discovery – A History. Wiley. pp. 260–261. ISBN 978-0-471-89980-8.
- ^ Weiss RA (May 1993). "How does HIV cause AIDS?". Science. 260 (5112): 1273–1279. Bibcode:1993Sci...260.1273W. doi:10.1126/science.8493571. PMID 8493571.
- ^ Douek DC, Roederer M, Koup RA (2009). "Emerging concepts in the immunopathogenesis of AIDS". Annual Review of Medicine. 60: 471–484. doi:10.1146/annurev.med.60.041807.123549. PMC 2716400. PMID 18947296.
- ^ NIH Clinical Center's 50th Anniversary. "Clinical Center 50th Anniversary Celebration" (PDF). Archived from the original (PDF) on June 19, 2013. Retrieved April 18, 2012.
- ^ Yarchoan R, Klecker RW, Weinhold KJ, Markham PD, Lyerly HK, Durack DT, Gelmann E, Lehrman SN, Blum RM, Barry DW (1986). "Administration of 3'-azido-3'-deoxythymidine, an inhibitor of HTLV-III/LAV replication, to patients with AIDS or AIDS-related complex". Lancet. 1 (8481): 575–80. doi:10.1016/s0140-6736(86)92808-4. PMID 2869302. S2CID 37985276.
- ^ "Did Controversial AZT Treatment Kill More Patients than AIDS in '80s, '90s?". September 21, 2021.
- ^ Fischl MA, Richman DD, Grieco MH, Gottlieb MS, Volberding PA, Laskin OL, et al. (July 1987). "The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. A double-blind, placebo-controlled trial". The New England Journal of Medicine. 317 (4): 185–191. doi:10.1056/NEJM198707233170401. PMID 3299089.
- ^ Brook I (September 1987). "Approval of zidovudine (AZT) for acquired immunodeficiency syndrome. A challenge to the medical and pharmaceutical communities". JAMA. 258 (11): 1517. doi:10.1001/jama.1987.03400110099035. PMID 3306004.
- ^ Cimons M (March 21, 1987). "U.S. Approves Sale of AZT to AIDS Patients". Los Angeles Times. p. 1.
- ^ AZT Approved for AIDS Children. "HEALTH : AZT Approved for AIDS Children". Los Angeles Times. May 3, 1990. Archived from the original on May 4, 2015. Retrieved March 30, 2012 – via From Times Wire Services.
- ^ "Zidovudine (AZT) | Johns Hopkins ABX Guide".
- ^ Greenhouse L (January 17, 1996). "Supreme Court Roundup;Justices Reject Challenge Of Patent for AIDS Drug". The New York Times. Archived from the original on November 17, 2016.
- ^ Armstrong M, Murphy Jr GM (April 26, 2012). "Inventorship and ownership considerations and pitfalls with collaborative research: patent highlight". ACS Medicinal Chemistry Letters. 3 (5): 349–51. doi:10.1021/ml300084e. PMC 4025834. PMID 24900477.
- ^ a b Meland M (May 3, 2004). "Judge Denies Request To Dismiss Patent Challenge Vs. Glaxo's AZT – Law360". Law360. Archived from the original on November 17, 2016.
- ^ "HIV/AIDS History of Approvals – HIV/AIDS Historical Time Line 2000 – 2010". U.S. Food and Drug Administration (FDA). August 8, 2014. Archived from the original on October 23, 2016.
External links
[edit]- "Zidovudine". Drug Information Portal. U.S. National Library of Medicine.
