Influenza
| Influenza | |
|---|---|
| Specialty | Family medicine, pulmonology, infectious diseases, emergency medicine |
| Influenza (flu) |
|---|
 |
Influenza, commonly known as the flu, is an infectious disease affecting birds and mammals and is caused by an RNA virus of the orthomyxoviridae family (the influenza viruses). The most common and characteristic symptoms of influenza in humans are fever, pharyngitis (sore throat), myalgia (muscle pains), severe headache, coughing, and malaise (weakness and fatigue).[1] In more serious cases, influenza can cause pneumonia and this can be fatal, particularly in young children or the elderly.
Influenza spreads rapidly by infected people sneezing and creating aerosols containing viruses. Flu spreads around the world in seasonal epidemics, killing millions of people in pandemic years and hundreds of thousands in nonpandemic years. Three influenza pandemics have occured in the 20th century, each following a major genetic change in the virus and have killed tens of millions of people. The world's current major influenza pandemic threat is H5N1; but it is at present mostly a flu in birds and has not yet mutated to spread between people.
A cold and a 'stomach flu' are very different from a flu. Influenza can be far more severe than the common cold and can even lead to death. Influenza and the common cold are caused by completely different viruses. Gastroenteritis is sometimes called "stomach flu" or "24 hour flu"; but that is a misnomer as it is not connected with influenza.
Etymology
The term influenza has its origins in 15th century Italy, where the cause of the disease was ascribed to unfavourable astrological influences. Evolution in medical thought led to its modification to "influenza di freddo", meaning "influence of the cold". The word "influenza" was first attested in English in 1743 when it was borrowed during an outbreak of the disease in Europe.[2]
History
Hippocrates first described the symptoms of influenza over two thousand years ago.[3] Since then, the virus has undergone mutations and shifts and has caused numerous pandemics. The first influenza pandemic was recorded in 1580 and investigations into influenza have continued since then.[4] The etiological cause of influenza, the orthomyxoviridae were finally discovered by the Medical Research Council (MRC) of the United Kingdom in 1933.[5]
Influenza pandemics are caused by antigenic shift, when two strains of influenza recombine forming a lethal new strain.[6] The most famous outbreak (and the most lethal) was the so-called Spanish Flu pandemic (type A influenza, H1N1 strain), which lasted from 1918 to 1919. The global mortality from the 1918/1919 pandemic is not known, but is estimated that 2.5 – 5% of the human population were killed, with 20% of the world population being infected. In this pandemic as many as 25 million may have been killed in the first 25 weeks; in contrast, HIV/AIDS has killed 25 million in its first 25 years. Influenza spread across the world, killing more than 25 million people in six months; some estimates put the total killed at over twice that number, possibly even 100 million.[7] Lesser flu epidemics included the 1957 Asian Flu (type A, H2N2 strain) and the 1968 Hong Kong Flu (type A, H3N2 strain).
| Name of pandemic | Date | Deaths | Strain involved |
|---|---|---|---|
| Asiatic (Russian) Flu | 1889-90 | 1 million | possibly H2N2 |
| Spanish Flu | 1918–20 | 40 million | H1N1 |
| Asian Flu | 1957–58 | 1 to 1.5 million | H2N2 |
| Hong Kong Flu | 1968–69 | 3/4 to 1 million | H3N2 |
Although there were scares in New Jersey in 1976 (the Swine Flu), worldwide in 1977 (the Russian Flu), and in Hong Kong (as well as in other Asian countries, namely continental China, as became known later) in 1997 (Avian influenza), there have been no major pandemics subsequent to the 1968 infection. Increased immunity from antibodies, and the development of flu vaccines have limited the spread of the virus, and may have helped prevent any further pandemics.[8]
Microbiology

Types of influenza virus
All influenza viruses are either Influenzavirus A, Influenzavirus B or Influenzavirus C.
Of these three types, the type A viruses are the most virulent human pathogens among the three influenza types and causes the most severe disease. The Influenza A virus can be subdivided inot different serotypes based on the antibody response to these viruses. The serotypes that have been confirmed in humans, ordered by the number of known human pandemic deaths, are:
- H1N1 caused "Spanish Flu"
- H2N2 caused "Asian Flu"
- H3N2 caused "Hong Kong Flu"
- H5N1 is the current pandemic threat
- H7N7 has unusual zoonotic potential
- H1N2 is currently endemic in humans and pigs
- H9N2, H7N2, H7N3, H10N7.
Influenza B virus almost exclusively infects humans, but usually causes comparitively mild symptoms. This type of influenza mutates at a rate 2-3 times lower than type A and consequently is less genetically diverse, with only one influenza B serotype.[9] Influenza C is less common than the other types and seems to cause disease mainly in children.[10]
- Influenza A
The following applies for Influenza A viruses:
Unusually for a virus, the influenza A genome is not a single piece of nucleic acid, instead it contains eight pieces of segmented negative-sense RNA, is 13.5 kilobases long and encodes 11 proteins (HA, NA, NP, M1, M2, NS1, NEP, PA, PB1, PB1-F2, PB2).[11] The best-characterised of these viral proteins are hemagglutinin and neuraminidase, two large glycoproteins found on the outside of the viral particles. Neuraminidase is an enzyme involved in the release of progeny virus from infected cells, by cleaving sugars that bind the mature viral particles: while hemagglutinin is a lectin that mediates binding of the virus to target cells.[12] The hemagglutinin (H) and neuraminidase (N) proteins are targets for antiviral drugs[13] and antibodies.[8] Their gene sequences are also used to name the different subtypes of influenza A viruses, hence the H and N in H5N1.
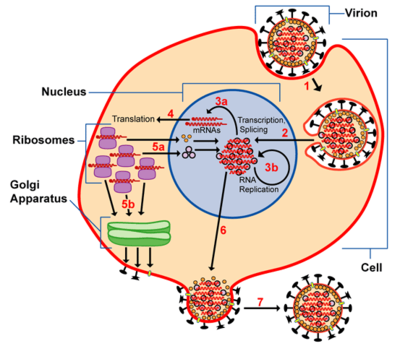
Infection and replication
The viruses bind to sialic acid sugars on the surface of epithelial cells through hemagglutinin (Stage 1 in infection figure).[14] The cell then takes in the virus by endocytosis. In the acidic endosome the viral envelope fuses with the vacuole's membrane: releasing the viral RNA (vRNA) molecules, accessory proteins and RNA-dependent RNA transcriptase into the cytoplasm (Stage 2). These proteins and vRNA move into the cell nucleus and the RNA-dependent RNA transcriptase begins transcribing complementary positive-sense vRNA (Steps 3a and b). The vRNA is either exported into the cytoplasm and translated (step 4), or remains in the nucleus. Newly-synthesised viral proteins are either secreted through the golgi apparatus onto the cell surface (in the case of neuraminidase and hemagglutinin, step 5b) or transported back into the nucleus to bind vRNA and form new viral genome particles (step 5a). Other viral proteins have multiple actions in the host cell, including degrading cellular mRNA and using the released nucleotides for vRNA synthesis and also inhibiting translation of host cell mRNAs.[15]
Negative-sense vRNAs which form the genomes of future viruses, RNA-dependent RNA transcriptase, and other viral proteins are assembled into a viral particle, or viron. Hemagglutinin and neuraminidase molecules cluster into a bulge in the cell membrane. The vRNA and viral core proteins leave the nucleus and enter this membrane protrusion (step 6). The mature virus then buds off from the cell in a sphere of host phospholipid membrane, thereby acquiring hemagglutinin and neuraminidase with this membrane coat (step 7). As before, the viruses adhere to the cell through hemagglutinin and it is only once neuraminidase has cleaved sialic acid residues from the host cell that the mature viruses can detach.[14] After the release of new influenza virus, the host cell dies.
Because of the absence of RNA proofreading enzymes, the RNA-dependent RNA transcriptase makes a single nucleotide insertion error per every 10 thousand nucleotides, which is the approximate length of the influenza vRNA. This makes nearly every newly-manufactured influenza virus a mutant.[16] Furthermore, the separation of the genome into eight separate segments of vRNA facilitates genetic recombination of the vRNAs and also mixing of vRNAs from different viral lines. The resulting rapid changes in viral genetics aids viral evolution to infect new host species or overcome protective immunity.[8]
Symptoms
Influenza's effects are much more severe than those of the "cold", and last longer. Recovery takes about one to two weeks. Influenza can be deadly, especially for the weak, old or chronically ill.[8] According to the on-line version of the Merck Manual of Diagnosis and Therapy:
- "Symptoms start 24 to 48 hours after infection and can begin suddenly. Chills or a chilly sensation are often the first indication of influenza. Fever is common during the first few days, and the temperature may rise to 102 to 103 °F (approximately 38 to 39 °C). Many people feel sufficiently ill to remain in bed for days; they have aches and pains throughout the body, most pronounced in the back and legs."[1]
The virus attacks the respiratory tract, is transmitted from person to person by saliva droplets expelled by coughing, and can cause the following symptoms:
Most people who get influenza will recover in one to two weeks, but others will develop life-threatening complications (such as pneumonia). Millions of people in the United States (about 10% to 20% of U.S. residents) are infected with influenza each year. An average of about 36,000 people per year in the United States die, and more than 200,000 per year are admitted to a hospital, as a result of influenza.[17] According to the World Health Organization: "Every winter, tens of millions of people get the flu. Most are home, sick and miserable, for about a week. Some—mostly the elderly—die. We know the worldwide death toll exceeds a few hundred thousand people a year, but even in developed countries the numbers are uncertain, because medical authorities don't usually verify who actually died of influenza and who died of a flu-like illness."[18] Even healthy people can be affected, and serious problems from influenza can happen at any age. People age 65 years and older, people of any age with chronic medical conditions, and very young children are more likely to get complications from influenza. Pneumonia, bronchitis, sinus, and ear infections are four examples of such complications.
The flu can make chronic health problems worse. For example, people with asthma may experience asthma attacks while they have the flu, and people with chronic congestive heart failure may have a worsening of this condition, that is triggered by the flu.
Many symptoms of the flu (fever, heart failure, headaches, lung damage and fatigue), are caused mainly by the huge production of proinflammatory cytokines and chemokines such as interferon or tumor necrosis factor from influenza-infected cells.[19][20] However, in contrast to the rhinovirus that causes the common cold, influenza does cause tissue damage, so symptoms are not entirely due to the inflammatory response.[21]
A CDC press release on January 7, 2003 said: "Using new and improved statistical models, CDC scientists estimate that an average of 36,000 people (up from 20,000 in previous estimates) die from influenza-related complications each year in the United States."[22]
Epidemiology
Influenza reaches peak prevalence in winter, and because the Northern and Southern Hemisphere have winter at different times of the year, there are actually two flu seasons each year. Therefore, the World Health Organization (assisted by the National Influenza Centers) makes two vaccine formulations every year; one for the Northern, and one for the Southern Hemisphere.[23]
It remains unclear why outbreaks of the flu occur seasonally rather than uniformly throughout the year. One possible explanation is that, because people are indoors more often during the winter, they are in close contact more often, and this promotes transmission from person to person. Another is that cold temperatures lead to drier air, which may dehydrate mucus, preventing the body from effectively expelling virus particles. The virus may also survive longer on exposed surfaces (doorknobs, countertops, etc.) in colder temperatures. Increased travel and visitation due to the Northern Hemisphere winter holiday season may also play a role.[24] However, seasonal changes in infection rates are also seen in tropical regions and these peaks of infection are seen mainly during the rainy season.[25] Seasonal changes in contact rates from school-terms, which are a major factor in other childhood diseases such as measles and pertussis, may also play a role in flu. A combination of these small seasonal effects may be amplified by "dynamical resonance" with the endogenous disease cycles.[26] The seasonality of H5N1 flu may provide important clues.
Prevention and treatment
Vaccination and hygiene

Vaccination against influenza with a flu vaccine is possible and in many cases recommended. These vaccines can be produced in several ways, the most common of these is the growth of the virus in hen eggs until it becomes avirulent. This egg-attenuated virus can then be mixed with a virulent serotype and the virus chemically inactivated by formalin or detergent treatment.[8]
The effectiveness of these flu vaccines are highly variable. Due to the high mutability of the virus, a particular flu vaccine formulation usually confers protection for no more than a few years. The World Health Organization predicts each year which strains of the virus that are most likely to be circulating in the next year, allowing pharmaceutical companies to develop vaccines that will provide immunity against these strains.
It is possible to get vaccinated and still get influenza. The vaccine is reformulated each season for a few specific flu strains, but cannot possibly include all the different strains actively infecting people in the world for that season. Also, it takes about six months for the manufacturers to formulate and produce the millions of doses required to deal with the seasonal epidemics; occasionally a new or overlooked strain becomes prominent during that six months and infects people even though they have been vaccinated (as in the 2003-2004 season).[27] It is also possible to get infected just before vaccination and still get sick with the very strain that the vaccine is supposed to prevent, as the vaccine will take a few days to become effective. The CDC says "About 2 weeks after vaccination, antibodies that provide protection against influenza virus infection develop in the body."[28]
Vaccination is most important in vulnerable populations, such as children or the elderly. The 2006-2007 season is the first in which the U.S. CDC has recommended that children (<59 months) receive the annual flu vaccine.[29] However, vaccines can cause the immune system to react as if the body were actually being infected, and general infection symptoms (many cold and flu symptoms are just general infection symptoms) can appear, though these symptoms are usually not as severe or as long-lasting as influenza.
The CDC says:
"The viruses in the flu shot are killed (inactivated), so you cannot get the flu from a flu shot. The risk of a flu shot causing serious harm, or death, is extremely small. However, a vaccine, like any medicine, may rarely cause serious problems, such as severe allergic reactions. Almost all people who get influenza vaccine have no serious problems from it."[30]
Personal health and hygiene are effective in avoiding and minimizing influenza. As influenza spreads through aerosols and contact with contaminated surfaces, persuading people to cover their mouths while sneezing and to wash their hands regularly, are particularly important.[29]
Treatment
- Main article Flu treatment contains curative treatments, symptom treatments and unconventional treatments such as antivirals, decongestants, and echinacea, respectively.
According to the CDC: Patients with the flu should get plenty of rest, drink a lot of liquids, avoid using alcohol and tobacco, and if desired then take medications such as acetaminophen to relieve the fever and muscle aches associated with the flu. Children and teenagers with flu symptoms (particularly fever) should avoid taking aspirin during an influenza infection (especially influenza type B) because doing so can lead to Reye syndrome, a rare but potentially fatal disease of the liver. [31]
The antiviral drugs amantadine and rimantadine block a viral ion channel and prevent the virus from infecting cells. These drugs are effective against influenza A if given early in the infection, but are ineffective against influenza B.[32] Antiviral drugs such as Oseltamivir (trade name Tamiflu) and Zanamivir are neuraminidase inhibitors that will halt the spread of the virus in the body.[33] These drugs are effective against both influenza A and B.[32]
Research
Influenza research includes molecular virology, pathogenesis, host immune responses, genomics, and epidemiology. These help in developing influenza countermeasures such as vaccines, therapies and diagnostic tools. Improved influenza countermeasures require this basic research on how viruses enter cells, replicate, mutate, evolve into new strains and induce an immune response. One particularly important basic research program is the Influenza Genome Sequencing Project, which is creating a library of influenza sequences that will help understand what makes one strain more lethal than another, what genetic determinants most affect immunogenicity, and how the virus evolves over time.[34]
Solutions to limitations in current vaccine methods are being researched. The US government has purchased from Sanofi Pasteur and Chiron Corporation several million doses of vaccine meant to be used in case of an influenza pandemic of H5N1 and is conducting clinical trials with these vaccines. [35] ABC News reported on April 1, 2006 that "Beginning in late 1997, the human trials have tested 30 different vaccines, all pegged to the H5N1 virus." [36]
Infection of other animals
 |
Influenza infects many animal species and transfer of viral strains between species can occur. However, waterfowl are thought to be the main reservoirs of influenza viruses.[37] Sixteen forms of hemagglutinin and 9 forms of neuraminidase have been identified. All known subtypes (HxNy) are found in birds but many subtypes are endemic in humans, dogs, horses, and pigs; populations of camels, ferrets, cats, seals, mink, and whales can also show evidence of prior infection or exposure to influenza.[37] Variants of flu virus are sometimes named according to the species the strain is endemic in or adapted to. The main variants named using this convention are: Bird flu, Human Flu, Swine Flu, Horse Flu and Dog Flu.
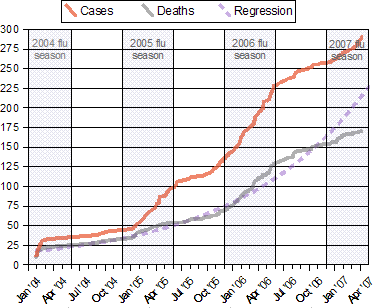
Influenza A virus subtype H5N1, also known as H5N1, is a subtype of the Influenza A virus that is capable of causing illness in many species, including humans.[38] An avian-adapted, highly pathogenic strain of H5N1 (called HPAI A(H5N1), for "highly pathogenic avian influenza virus of type A of subtype H5N1") is the causative agent of H5N1 flu, commonly known as "avian influenza" or simply "bird flu", and is endemic in many bird populations, especially in Southeast Asia. This Asian lineage strain of HPAI A(H5N1) is spreading globally. It is epizootic (an epidemic in nonhumans) and panzootic (a disease affecting animals of many species, especially over a wide area) killing tens of millions of birds and spurring the culling of hundreds of millions of other birds in an attempt to control its spread. Most references in the media to "bird flu" and most references to H5N1 are about this specific strain.[39][40]
HPAI A(H5N1) is an avian disease and there is no evidence suggesting either efficient human-to-human transmission of HPAI A(H5N1) or of airborne transmission to humans. Those infected with H5N1 have had, in almost all cases, extensive physical contact with infected birds. However, H5N1 may in the future mutate or reassort into a strain capable of efficient human-to-human transmission. Due to the high lethality and virulence of human HPAI A(H5N1) infection to date, its endemic presence, its large and increasing biological host reservoir, and its significant ongoing mutations, the H5N1 virus is today the world's major current pandemic threat, and billions of dollars are being raised and spent researching H5N1 and preparing for a potential influenza pandemic.[41]
Flu symptoms in birds are variable and symptoms can be fairly unspecific.[42] The symptoms following infection with low-pathogenicity avian influenza may be as simple as ruffled feathers, a small reduction in egg production or weight loss combined with minor respiratory disease.[43] These mild symptoms can make diagnosos in the field difficult, so tracking the spread of avian influenza requires laboratory testing of samples from infected birds. However, some strains such as Asian H9N2 or H5N1 are highly virulent to poultry, and may cause more extreme symptoms and significant mortality.[44] For example, in its most highly pathogenic form, influenza in chickens and turkeys produces a sudden appearance of severe symptoms and almost 100 % mortality within two days.[45]
See also
References
- ^ a b Influenza: Viral Infections: Merck Manual Home Edition
- ^ etymonline.com On-line etymology dictionary by Douglas Harper
- ^ "Of the Epidemics" By Hippocrates, written 400 B.C.E and Translated by Francis Adams. Accessed 18 Oct 06.
- ^
Webster, R. G. and Walker, E. J. (2003). "The world is teetering on the edge of a pandemic that could kill a large fraction of the human population". American Scientist. 91 (2): 122. doi:10.1511/2003.2.122.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Blakemore, C. "Battle of time, luck and science" The Sunday Times - Britain 20-04-09. Accessed 22 June 06
- ^ Scholtissek C. "Molecular epidemiology of influenza." Arch Virol Suppl. 1997;13:99-103. PMID 9413530
- ^ Forum on Microbial Threats Board on Global Health: Knobler SL, Mack A, Mahmoud A, Lemon SM. (ed.) The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005). Washington DC: The National Academies Press. Chapter 1 p57.
- ^ a b c d e f Hilleman MR. "Realities and enigmas of human viral influenza: pathogenesis, epidemiology and control." Vaccine. 2002 Aug 19;20(25-26):3068-87. PMID 12163258
- ^ Hay AJ, Gregory V, Douglas AR, Lin YP. "The evolution of human influenza viruses." Philos Trans R Soc Lond B Biol Sci. 2001 Dec 29;356(1416):1861-70. PMID 11779385
- ^ Matsuzaki Y, Katsushima N, Nagai Y, Shoji M, Itagaki T, Sakamoto M, Kitaoka S, Mizuta K, Nishimura H. "Clinical features of influenza C virus infection in children." J Infect Dis. 2006 May 1;193(9):1229-35. PMID 16586359
- ^ Ghedin E, Sengamalay NA, Shumway M, Zaborsky J, Feldblyum T, Subbu V, Spiro DJ, Sitz J, Koo H, Bolotov P, Dernovoy D, Tatusova T, Bao Y, St George K, Taylor J, Lipman DJ, Fraser CM, Taubenberger JK, Salzberg SL. "Large-scale sequencing of human influenza reveals the dynamic nature of viral genome evolution." Nature. 2005 Oct 20;437(7062):1162-6. PMID 16208317
- ^ Couch, R. "Medical Microbiology" Chapter 58. Orthomyxoviruses Multiplication 1996 The University of Texas Medical Branch at Galveston ISBN 0-9631172-1-1
- ^ Wilson JC, von Itzstein M. "Recent strategies in the search for new anti-influenza therapies." Curr Drug Targets. 2003 Jul;4(5):389-408. PMID 12816348
- ^ a b Wagner R, Matrosovich M, Klenk HD. "Functional balance between haemagglutinin and neuraminidase in influenza virus infections." Rev Med Virol. 2002 May-Jun;12(3):159-66. PMID 11987141
- ^ Kash JC, Goodman AG, Korth MJ, Katze MG. "Hijacking of the host-cell response and translational control during influenza virus infection." Virus Res. 2006 Jul;119(1):111-20. PMID 16630668
- ^ Drake JW. "Rates of spontaneous mutation among RNA viruses." Proc Natl Acad Sci U S A. 1993 May 1;90(9):4171-5. PMID 8387212
- ^ National Strategy for Pandemic Influenza November 1, 2005
- ^ Peter M. Sandman and Jody Lanard "Bird Flu: Communicating the Risk" 2005 Perspectives in Health Magazine Vol. 10 issue 2.
- ^ Calabrese F, Carturan E, Chimenti C, Pieroni M, Agostini C, Angelini A, Crosato M, Valente M, Boffa GM, Frustaci A, Thiene G. "Overexpression of tumor necrosis factor (TNF)alpha and TNFalpha receptor I in human viral myocarditis: clinicopathologic correlations." Mod Pathol. 2004 Sep;17(9):1108-18. PMID 15218506
- ^ Schmitz N, Kurrer M, Bachmann MF, Kopf M. "Interleukin-1 is responsible for acute lung immunopathology but increases survival of respiratory influenza virus infection." J Virol. 2005 May;79(10):6441-8. PMID 15858027
- ^ Winther B, Gwaltney JM Jr, Mygind N, Hendley JO. "Viral-induced rhinitis." Am J Rhinol. 1998 Jan-Feb;12(1):17-20. PMID 9513654
- ^ CDC Press release January 7, 2003 CDC Finds Annual Flu Deaths Higher Than Previously Estimated
- ^ Recommended composition of influenza virus vaccines for use in the 2006–2007 influenza season WHO report 2006-02-14. Accessed 19 Oct 06.
- ^ Weather and the Flu Season NPR Day to Day, December 17, 2003. Accessed, 19 Oct 06
- ^ Shek LP, Lee BW. "Epidemiology and seasonality of respiratory tract virus infections in the tropics." Paediatr Respir Rev. 2003 Jun;4(2):105-11. PMID 12758047
- ^ Dushoff J, Plotkin JB, Levin SA, Earn DJ. "Dynamical resonance can account for seasonality of influenza epidemics." Proc Natl Acad Sci U S A. 2004 Nov 30;101(48):16915-6. PMID 15557003
- ^ Holmes EC, Ghedin E, Miller N, Taylor J, Bao Y, St George K, Grenfell BT, Salzberg SL, Fraser CM, Lipman DJ, Taubenberger JK. "Whole-genome analysis of human influenza A virus reveals multiple persistent lineages and reassortment among recent H3N2 viruses." PLoS Biol. 2005 Sep;3(9):e300. PMID 16026181
- ^ Key Facts about Influenza (Flu) Vaccine CDC publication October 17, 2006. Accessed 18 Oct 06.
- ^ a b Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP) CDC report (MMWR 2006 Jul 28;55(RR10):1-42) Accessed 19 Oct 06.
- ^ Questions & Answers: Flu Shot CDC publication Updated Jul 24, 2006. Accessed 19 Oct 06.
- ^ Glasgow JF, Middleton B. "Reye syndrome--insights on causation and prognosis." Arch Dis Child. 2001 Nov;85(5):351-3. PMID 11668090
- ^ a b Stephenson I, Nicholson KG. "Chemotherapeutic control of influenza." J Antimicrob Chemother. 1999 Jul;44(1):6-10. PMID 10459804
- ^ Moscona A. "Neuraminidase inhibitors for influenza." N Engl J Med. 2005 Sep 29;353(13):1363-73. PMID 16192481
- ^ Influenza A Virus Genome Project at The Institute of Genomic Research. Accessed 19 Oct 06
- ^ New York Times article ""Doubt Cast on Stockpile of a Vaccine for Bird Flu"" by Denise Grady. Published: March 30, 2006. Accessed 19 Oct 06
- ^ In Bird Flu Vaccine Hunt, 1976 Tragedy Looms ABC news April 1, 2006. Accessed Oct 19 2006
- ^ a b Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. "Evolution and ecology of influenza A viruses." Microbiol Rev. 1992 Mar;56(1):152-79. PMID 1579108
- ^ International Committee on Taxonomy of Viruses 2002 46.0.1. Influenzavirus A Accessed 17 April 2006
- ^ Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. "Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia" Nature 2004;430(6996), 209-13 PMID 15241415
- ^ Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. "The Threat of Pandemic Influenza: Are We Ready?" Workshop Summary The National Academies Press (2005) "Today's Pandemic Threat: Genesis of a Highly Pathogenic and Potentially Pandemic H5N1 Influenza Virus in Eastern Asia", pages 116-130
- ^ Rosenthal, E. and Bradsher, K. Is Business Ready for a Flu Pandemic? The New York Times 16-03-2006 Accessed 17-04-2006
- ^ Elbers AR, Koch G, Bouma A. "Performance of clinical signs in poultry for the detection of outbreaks during the avian influenza A (H7N7) epidemic in The Netherlands in 2003." Avian Pathol. 2005 Jun;34(3):181-7. PMID 16191700
- ^ Capua I, Mutinelli F. "Low pathogenicity (LPAI) and highly pathogenic (HPAI) avian influenza in turkeys and chicken." In: Capua I, Mutinelli F. (eds.), A Colour Atlas and Text on Avian Influenza, Papi Editore, Bologna, 2001, pp. 13-20
- ^ Bano S, Naeem K, Malik SA. "Evaluation of pathogenic potential of avian influenza virus serotype H9N2 in chickens." Avian Dis. 2003;47(3 Suppl):817-22. PMID 14575070
- ^ Swayne DE, Suarez DL. "Highly pathogenic avian influenza." Rev Sci Tech. 2000 Aug;19(2):463-82.PMID 10935274
Further reading
- Special Issue: Influenza (>20 articles). Emerging Infectious Diseases, January 2006.
- CDC 2005. Centers for Disease Control. Prevention and Control of Influenza Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2005; 54 (RR08): 1-40. - Full text.
- CDC info on influenza
- World Health Organization Fact Sheet Overview of influenza.
- NHS Direct Health encyclopedia entry
- BioHealthBase Bioinformatics Resource Center Database of influenza sequences and related information.
- Influenza Report 2006 Online book. Research level information. Highly recommended.
- Medicine Net's overview of influenza
- Congressional Research Service (CRS) Reports regarding Influenza Law related government reports.
- Influenza Surveillance and Contingency Plans (by Country/Region)
- Orthomyxoviridae The Universal Virus Database of the International Committee on Taxonomy of Viruses.
- Influenza Virus Resource from the NCBI.
- 'Myxoviruses' Microbiology at the University of Leicester.
