Mumps virus
| Mumps orthorubulavirus | |
|---|---|
| |
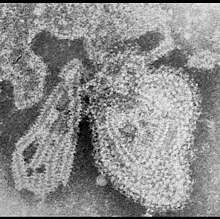
| TEM micrograph of a Mumps orthorubulavirus particle | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Monjiviricetes |
| Order: | Mononegavirales |
| Family: | Paramyxoviridae |
| Genus: | Orthorubulavirus |
| Species: | Mumps orthorubulavirus
|
| Synonyms[1] | |
| |
The mumps virus (MuV), scientific name Mumps orthorubulavirus, is the virus that causes mumps. MuV contains a negative-sense genome made of ribonucleic acid (RNA) that encodes seven genes containing nine proteins. It is pleomorphic in shape, 100 to 600 nanometers in diameter, and consists of its genome surrounded by a capsid that is in turn surrounded by a viral envelope. Twelve genotypes are recognized, which vary in their geographic distribution. In comparison to other RNA viruses, MuV has a very low mutation rate.
Humans are the only natural host of the mumps virus. Infection is characterized by inflammation of the parotid glands in front of the ears. Symptoms usually self-reslove within a few weeks but long-term complications can occur. Infection is preventable with vaccines. MuV contains various mechanisms to counteract the immune system, which seems to have an inherently weak response to the mumps virus.
The mumps virus was first identified as the cause of mumps in 1934 and was first isolated in 1945. Within a few years after isolation, vaccines protecting against MuV infection had been developed. MuV was first recognized as a species in 1971. It is the type species of the genus Orthorubulavirus in the subfamily Rubulavirinae, family Paramyxoviridae.
Characteristics
Genome
The mumps virus contains a nonsegmented, linear genome that is 15,384 nucleotides in length and made of ribonucleic acid (RNA). The genome has negative sense so that messenger RNA (mRNA) can be transcribed directly from the genome. Mumps virus encodes seven genes in the following order:[2][3][4]
- nucleo- (N) protein,
- V/P/I (V/phospho-(P)/I) proteins,
- matrix (M) protein, the most abundant protein in virions,[5]
- fusion (F) protein,
- small hydrophobic (SH) transmembrane protein,
- hemagglutinin-neuraminidase (HN), and
- the large (L) protein.
The L and P proteins combine to form the RNA-dependent RNA polymerase (RdRp). RdRp acts as both a replicase to replicate the genome and as a transcriptase to transcribe mRNA from the genome. Unlike the other proteins, the I protein's function is unknown.[2]
Structure
The genome of the mumps virus is encased by N proteins to form a flexible, loosely coiled helical ribonucleoprotein (RNP) complex consisting of the genome surrounded by a nucleocapsid that RdRp is bound to. RNPs are surrounded by an envelope, a lipid membrane, which contains two types of spikes on its surface that correspond to the HN and F glycoproteins. M proteins are found on the inner side of the envelope, connecting the envelope to the RNP. Virions vary in size from 100 to 600 nanometers (nm) in diameter and are pleomorphic in shape.[2][5][6]
Life cycle
MuV first interacts with a host cell by binding to its surface via the HN protein's receptor, sialic acid, which binds to sialic acid receptors on the surface of host cells. Following attachment, the F protein is triggered and begins fusing the viral envelope with the host cell's membrane. The F protein does so by changing from a metastable state to refolding to a more stable hairpin structure, which allows the contents of the virion, including the RNP, to be released into the host cell's cytoplasm.[2][5][6]
Upon entering the host cell, the RdRp begins transcring mRNA from the genome inside the RNP. Transcription starts at or near the 3'-end (usually pronounced "three prime end") at a promoter region and moves sequentially toward the 5'-end. One mRNA strand is transcribed for each gene, and it is necessary for all genes sequentially before a gene to be transcribed for that gene to be transcribed. Genes closer to the 3'-end are transcribed at the highest frequency, decreasing in frequency as RdRp approaches the 5'-end. RdRp synthesizes a cap on the 5'-end of the mRNA and a polyadenylated tail on the 3'-end consisting of hundreds of consecutive adenines. Once a gene has been transcribed, RdRp releases it into the cytoplasm for subsequent translation of viral proteins by host ribosomes.[2][6][7][8] The V and P proteins are encoded by the same gene, so while transcribing mRNA, RdRp edits the mRNA by inserting two non-templated guanines into the mRNA to transcribes mRNA for the P protein.[9]
Later in the replication cycle, once a sufficient number of nucleoproteins are present after translation, RdRp switches functions to replicate the genome. This occurs in a two-step process: first, a positive-sense antigenome is synthesized by RdRp from the negative-sense genome, and second, negative-sense genomic RNA strands are in turn synthesized by RdRp from the antigenome. During this process, the antigenome and newly replicated genomes are encapsidated by the nucleoprotein at the same time as replication.[2][6][8] Progeny genomes can be used for additional transcription or replication or may simply be packaged into progeny virions.[5]
HN and F proteins are synthesized in the endoplasmic reticulum and travel through the Golgi complex to the cell membrane, whether they bind to the cell membrane and protrude from the surface of the cell. M proteins bind to the sites of the cell membrane where HN and F proteins are, doing so at the positions where their "tails" protrude into the inside of the cell membrane in the cytoplasm. M proteins then act as a signals to newly synthesized RNPs as to where virions are to be formed. The interaction of RNP and M proteins is then thought to trigger budding from the host cell.[2][5][6][10]
Budding from the host cell begins once M proteins recruit host class E proteins that form endosomal sorting complex required for transport (ESCRT) structures at the site of budding. There, ESCRT proteins form into concentric spirals and push the contents of the virion outward from the cell in the form of a vesicle that protrudes from the cell. The ESCRT proteins then constrict the opening of the vesicle and terminate budding by cutting off the vesicle from the rest of the membrane, forming a complete virion that is released from the host cell.[5][10][11] During this process, the neuraminidase of HN proteins aid in separation from the host membrane and prevent virion aggregation.[6]
Diversity
The mumps virus has one serotype and twelve genotypes. The genotypes can be distinguished based on the F, SH, are HN genes. The SH gene has a degree of variation between genotypes ranging from 5% to 21%, the highest among MuV's genes. The genotypes are named genotypes A to N, excluding E and M, i.e. genotypes A, B, C, D, F, G, H, I, J, K, L, and N. Genotypes E and M were previously recognized but were abolished due to phylogenetic analysis that MuVs assigned to them instead belonged genotypes C and K, respectively.[12][13]
The different genotypes vary in their geographic distribution. For example, genotypes C, D, H, and J are common in the western hemisphere, whereas genotypes F, G, and I are more common in Asia, although genotype G is considered to be a global genotype. Genotypes A and B have not been observed in the wild since the 1990s. This diversity of MuV is not reflected in the antibody response since because there is only one serotype, antibodies to one genotype are also functional against all others.[14]
Evolution
The F, SH, HN genes, used to distinguish genotypes, are estimated to experience genetic mutations at a rate of 0.25 · 10−3 substitutions per site per year, which is considered to be a very low mutation rate for an RNA virus.[13][15][16][17] Phylogenetic analysis of the entire SH gene indicates that genotypes A and J are related in one branch and split apart from the other genotypes. In that second branch, genotype I is a sister clade of the other genotypes, which cluster into five sequential sister clades: G and H; D and K; C; L; and B, F, and N.[12]
Immune system interactions
The SH protein is thought to be involved in blocking NF(α)-mediated apoptosis of the host cell, which is done as an antiviral response to suppress the spread of viruses, though SH is not necessary for replication since MuVs engineered without SH are still able to replicate. The V protein is also involved in evading host antiviral responses, by which it inhibits production and signalling of interferons.[2]
The immune system's reaction to MuV seems inherently weak for several reasons. Infections can occur in vaccinated individuals, which may be because memory T lymphocytes are necessary but inadequate for protection. In in vitro studies, there is usually a low concentration of antibodies against the virus, which mostly appear directed to the nucleoprotein, which does not neutralize infection since only antibodies that target NH receptors are protective.[14] Lastly, mumps-specific memory B lymphocytes have been reported to be low in frequency, possibly due to a low abundance of viral proteins during infection or an inadequate response by T cells.[18]
Classification
Mumps virus, scientific name Mumps orthorubulavirus, is the type species of the genus Orthorubulavirus, in the subfamily Rubulavirinae, family Paramyxoviridae.[1] Strains of MuV are named and classified using the the following system:[12]
- MuVs (RNA sequence derived from clinical material) or MuVi (RNA sequence derived from cell culture)
- City.Country ISO3 code
- Week number.year, the date of onset of when the disease occurred, or the date of specimen collection if the disease onset date is unknown, or the date the sample was received in the laboratory if the two prior dates are unknown
- replicate in week
- [genotype], which indicates which genotype the strain belongs to
- (VAC), which is used to indicate strains derived from cases with a history of vaccination and with vaccine virus detected
This system is used in sequential order. For example, MuVs/NewYork.USA/17.11[B] (VAC) is a vaccine-associated genotype B MuV derived from clinical material in New York City, and MuVi/London.GBR/3.12/2[G] is a genotype G MuV derived from cell culture in London.[12]
Disease
Humans are the only natural host of the mumps virus, which causes mumps. The disease is transmitted via contact with respiratory secretions such as aerosolized droplets and saliva. Infection leads to fever, muscle pain, and painful swelling of the parotid glands, two salivary glands situated on the sides of the mouth in front of the ears. Infection may also involve many other tissues and organs, resulting in a variety of inflammatory reactions such as encephalitis, aseptic[19] meningitis, orchitis, myocarditis, pancreatitis, nephritis, oophoritis, and mastitis. Mumps is usually benign and resolves within a few weeks after the onset of symptoms, but long-term complications such as paralysis, seizures, hydrocephalus, and deafness can occur. Treatment is supportive in nature, and infection is preventable via vaccination.[2][18][20]
History
The earliest known written account of mumps was in the 5th century B.C. by Greek physician Hippocrates. He described an outbreak of mumps on the island of Thasos in approximately 410 B.C. and provided a fuller description of the disease in Corpus Hippocraticum in Epidemics. In 1934, the etiology of the disease, the mumps virus, was discovered by Claude D. Johnson and Ernest William Goodpasture. They found that rhesus macaques exposed to saliva taken from humans in the early stages of the disease developed mumps. Furthermore, they showed that mumps could then be transferred to children via filtered and sterilized, bacteria-less preparations of macerated monkey parotid tissue, showing that it was a viral disease.[2][21]
The mumps virus was isolated for the first time in 1945 and by 1948 the first mumps vaccine had been developed. This vaccine contained inactivated virus particles and provided short-term protection against mumps. In the 1960s, Maurice Hilleman developed a more effective mumps vaccine using live virus particles that were taken from his then five-year-old infected daughter, Jeryl Lynn. This vaccine was approved for use in 1967 and recommended in 1977, replacing prior vaccines that were less effective. Hilleman would also work to develop the MMR vaccine in 1971, effective against measles, mumps, and rubella. The "Jeryl Lynn" strain of the mumps virus, which belongs to genotype A,[14] continues to be used in vaccines against mumps.[21]
Mumps virus was recognized as a species in 1971 by the International Committee on Taxonomy of Viruses (ICTV), which oversees virus taxonomy, when it was assigned to the genus Paramyxovirus. Since then, it has undergone numerous taxonomic changes and changes to its scientific name:[1][22]
- In 1995, Mumps virus was established as the type species of the newly established genus Rubulavirus.
- In 2016, Mumps virus was renamed to Mumps rubulavirus.
- In 2018, Mumps rubulavirus was renamed to Mumps orthorubulavirus to accompany Rubulavirus being abolished and replaced with the subfamily Rubulavirinae bearing the same name and the newly established genus Orthorubulavirus.
Etymology
The word "mumps" is first attested circa 1600 and is the plural form of "mump", meaning "grimace", originally a verb meaning "to whine or mutter like a beggar". The disease was likely called mumps in reference to the swelling caused by mumps parotitis, reflecting its impact on facial expressions as well as its causing of painful, difficult swallowing. "Mumps" as also used starting from the 17th century to mean "a fit of melancholy, sullenness, silent displeasure".[19][23]
References
- ^ a b c "ICTV Taxonomy history: Mumps orthorubulavirus". International Committee on Taxonomy of Viruses. International Committee on Taxonomy of Viruses. Retrieved 21 August 2020.
- ^ a b c d e f g h i j Rubin S, Eckhaus M, Rennick LJ, Bamford CG, Duprex WP (January 2015). "Molecular biology, pathogenesis and pathology of mumps virus". J Pathol. 235 (2): 242–252. doi:10.1002/path.4445. PMC 4268314. PMID 25229387. Retrieved 21 August 2020.
- ^ Cox RM, Plemper RK (June 2017). "Structure and organization of paramyxovirus particles". Curr Opin Virol. 24: 105–114. doi:10.1016/j.coviro.2017.05.004. PMC 5529233. PMID 28601688.
- ^ Rima B, Buschmann AB, Dundon WG, Duprex P, Easton A, Fouchier R, Kurath G, Lamb R, Lee B, Rota P, Wang L (December 2019). "ICTV Virus Taxonomy Profile: Paramyxoviridae". J Gen Virol. 100 (12): 1593–1954. doi:10.1099/jgv.0.001328. PMC 7273325. PMID 31609197. Retrieved 21 August 2020.
- ^ a b c d e f Najjar FE, Schmitt AP, Dutch RE (7 August 2014). "Paramyxovirus glycoprotein incorporation, assembly and budding: a three way dance for infectious particle production". Viruses. 6 (8): 3019–3054. doi:10.3390/v6083019. PMC 4147685. PMID 25105277. Retrieved 21 August 2020.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f Harrison MS, Sakaguchi T, Schmitt AP (September 2010). "Paramyxovirus assembly and budding: building particles that transmit infections". Int J Biochem Cell Biol. 42 (9): 1416–1429. doi:10.1016/j.biocel.2010.04.005. PMC 2910131. PMID 20398786.
- ^ Barr JN, Tang X, Hinzman E, Shen R, Wertz GW (10 May 2008). "The VSV polymerase can initiate at mRNA start sites located either up or downstream of a transcription termination signal but size of the intervening intergenic region affects efficiency of initiation". Virology. 374 (2): 261–270. doi:10.1016/j.virol.2007.12.023. PMC 2593140. PMID 18241907.
- ^ a b "Paramyxoviridae". ViralZone. Swiss Institute of Bioinformatics. Retrieved 21 August 2020.
- ^ Berg M, Hjertner B, Moreno-Lopez J, Linne T (May 1992). "The P gene of the porcine paramyxovirus LPMV encodes three possible polypeptides P, V and C: the P protein mRNA is edited". J Gen Virol. 73 (5): 1195–1200. doi:10.1099/0022-1317-73-5-1195. PMID 1588322.
- ^ a b Li M, Schmitt PT, Li Z, McCrory TS, He B, Schmitt AP (July 2009). "Mumps virus matrix, fusion, and nucleocapsid proteins cooperate for efficient production of virus-like particles". J Virol. 83 (14): 7261–7272. doi:10.1128/JVI.00421-09. PMC 2704775. PMID 19439476. Retrieved 21 August 2020.
- ^ "Viral budding via the host ESCRT complexes". ViralZone. Swiss Institute of Bioinformatics. Retrieved 21 August 2020.
- ^ a b c d "Mumps virus nomenclature update: 2012" (PDF). Wkly Epidemiol Rec. 87 (22): 217–224. 1 June 2012. PMID 24340404. Retrieved 21 August 2020.
- ^ a b Soetenes L, Backer JA, Hahne S, Binnendijk RV, Gouma S, Wallinga J (March 2019). "Visual tools to assess the plausibility of algorithm-identified infectious disease clusters: an application to mumps data from the Netherlands dating from January 2009 to June 2016". Euro Surveill. 24 (12): 1800331. doi:10.2807/1560-7917.ES.2019.24.12.1800331. PMC 6440581. PMID 30914076. Retrieved 21 August 2020.
- ^ a b c Beleni AI, Borgmann S (31 July 2018). "Mumps in the Vaccination Age: Global Epidemiology and the Situation in Germany". Int J Environ Res Public Health. 15 (8): 1618. doi:10.3390/ijerph15081618. PMC 6121553. PMID 30065192. Retrieved 21 August 2020.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Cui A, Rivailler P, Zhu Z, Deng X, Hu Y, Wang Y, Li F, Sun Z, He J, Si Y, Tian X, Zhou S, Lei Y, Zheng H, Rota PA, Xu W (7 December 2017). "Evolutionary analysis of mumps viruses of genotype F collected in mainland China in 2001-2015". Sci Rep. 7 (1): 17144. doi:10.1038/s41598-017-17474-z. PMC 5719434. PMID 29215070. Retrieved 21 August 2020.
- ^ Cui A, Rivailler P, Zhu Z, Deng X, Hu Y, Wang Y, Li F, Sun Z, He J, Si Y, Tian X, Zhou S, Lei Y, Zheng H, Rota PA, Xu W (7 December 2017). "Evolutionary analysis of mumps viruses of genotype F collected in mainland China in 2001-2015". Sci Rep. 7 (1): 17144. doi:10.1038/s41598-017-17474-z. PMC 5719434. PMID 29215070. Retrieved 21 August 2020.
- ^ Jenkins GM, Rambaut A, Pybus OG, Holmes EC (7 December 2017). "Rates of molecular evolution in RNA viruses: a quantitative phylogenetic analysis". J Mol Evol. 54 (2): 156–165. doi:10.1007/s00239-001-0064-3. PMID 11821909.
- ^ a b Latner DR, Hickman CJ (7 May 2015). "Remembering mumps". PLoS Pathog. 11 (5): e1004791. doi:10.1371/journal.ppat.1004791. PMC 4423963. PMID 25951183. Retrieved 21 August 2020.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Davis NF, McGuire BB, Mahon JA, Smyth AE, O'Malley KJ, Fitzpatrick JM (April 2010). "The increasing incidence of mumps orchitis: a comprehensive review". BJU Int. 105 (8): 1060–1065. doi:10.1111/j.1464-410X.2009.09148.x. PMID 20070300. Retrieved 21 August 2020.
- ^ Ramanathan R, Voigt EA, Kennedy RB, Poland GA (18 June 2018). "Knowledge gaps persist and hinder progress in eliminating mumps". Vaccine. 36 (26): 3721–3726. doi:10.1016/j.vaccine.2018.05.067. PMC 6031229. PMID 29784466.
- ^ a b "Tracing the story of mumps: a timeline". Pharmaceutical Technology. Pharamaceutical Technology. Retrieved 21 August 2020.
- ^ Buschmann AB, Dundon WG, Easton AJ, Fouchier RA, Kurath G, Lamb RA, Rima BK, Rota PA, Wang L (6 June 2018). "Re-organization of the family Paramyxoviridae" (docx). International Committee on Taxonomy of Viruses. Retrieved 21 August 2020.
- ^ "mumps (n.)". Etymonline. Online Etymology Dictionary. Retrieved 21 August 2020.
