Snakebite: Difference between revisions
DendroNaja (talk | contribs) |
DendroNaja (talk | contribs) |
||
| Line 138: | Line 138: | ||
==Snakes of particular concern== |
==Snakes of particular concern== |
||
===Black mamba and Coastal taipan=== |
===Black mamba and Coastal taipan=== |
||
[[File:Dendroaspis polylepis by Bill Love.jpg|left|thumb| |
[[File:Dendroaspis polylepis by Bill Love.jpg|left|thumb|120px|Black mamba]] |
||
[[Image:Coastal-Taipan.jpg|thumb|right| |
[[Image:Coastal-Taipan.jpg|thumb|right|160px|Coastal taipan]] |
||
Clinical mortality rate (often determined by measured toxicity on mice) is a commonly used indicator to determine the danger of any given venomous snake, but important too are its efficiency of venom delivery, its venom yield and its behavior when it encounters humans. Black mambas in particular are known to be high-strung, are the fastest snake species in the world, are highly aggressive, defensive and they are well known to have an irascible temperament.<ref name=NG>{{cite web|title=Black Mamba|url=http://animals.nationalgeographic.com/animals/reptiles/black-mamba/|work=National Geographic|publisher=National Geographic|accessdate=20 October 2013}}</ref><ref name=NW>{{cite book|last=White|first=Nancy|title=Black Mambas: Sudden Death!|year=2009|publisher=Bearport Publishing|isbn=1597167665}}</ref> Black mambas are also known to be the most accurate strikers, usually striking several times in quick succession. They are also known to have a 100% rate of envenomation. The probability of dry bites (no venom injected) in black mamba strikes is almost non-existent.<ref name='Davidson'/><ref name=Crisp>{{cite journal|last=Crisp|first=NG|title=Black mamba envenomation|journal=South African Medical Journal|date=31|year=1985|month=August|volume=68|issue=5|pages=293-4|pmid=4035489|accessdate=20 October 2013}}</ref> To date there has been no reported case of confirmed and medically treated black mamba bite in children.<ref name=Hilligan>{{cite journal|last=Hilligan|first=R|title=Black mamba bites. A report of 2 cases|journal=South African Medical Journal|date=1|year=1987|month=August|volume=72|issue=3|pages=220-1|pmid=3603321|url=http://www.ncbi.nlm.nih.gov/pubmed/3603321|accessdate=20 October 2013}}</ref> Coastal taipans can also be quite aggressive when cornered and will actively defend themselves.<ref name="DD"/> Untreated [[black mamba]] (''Dendroaspis polylepis'') and [[coastal taipan]] (''Oxyuranus scutellatus'') bites have a mortality rate of 100%.<ref name='Davidson'>{{cite web|url=http://drdavidson.ucsd.edu/portals/0/snake/dendroa3.htm|title=IMMEDIATE FIRST AID|last=Davidson|first=Terence|publisher=University of California, San Diego}}</ref><ref name="DD">{{cite web|url= http://drdavidson.ucsd.edu/Portals/0/snake/Oxyura~2.htm|title= IMMEDIATE FIRST AID for bites by Australian taipan or common taipan}}</ref> Black mamba and coastal taipan bites require very rapid and vigorous antivenom therapy as they are almost always fatal. The venoms of both species are exceptionally quick acting and both can cause human fatality in as little as 15-30 minutes. Black mambas in particular have been known to cause death in as little as 20 minutes post-envenomation.<ref name=NG/><ref name=NW/> These two snake species are generally accepted to be the deadliest snakes in the world by most herpetologists. |
Clinical mortality rate (often determined by measured toxicity on mice) is a commonly used indicator to determine the danger of any given venomous snake, but important too are its efficiency of venom delivery, its venom yield and its behavior when it encounters humans. Black mambas in particular are known to be high-strung, are the fastest snake species in the world, are highly aggressive, defensive and they are well known to have an irascible temperament.<ref name=NG>{{cite web|title=Black Mamba|url=http://animals.nationalgeographic.com/animals/reptiles/black-mamba/|work=National Geographic|publisher=National Geographic|accessdate=20 October 2013}}</ref><ref name=NW>{{cite book|last=White|first=Nancy|title=Black Mambas: Sudden Death!|year=2009|publisher=Bearport Publishing|isbn=1597167665}}</ref> Black mambas are also known to be the most accurate strikers, usually striking several times in quick succession. They are also known to have a 100% rate of envenomation. The probability of dry bites (no venom injected) in black mamba strikes is almost non-existent.<ref name='Davidson'/><ref name=Crisp>{{cite journal|last=Crisp|first=NG|title=Black mamba envenomation|journal=South African Medical Journal|date=31|year=1985|month=August|volume=68|issue=5|pages=293-4|pmid=4035489|accessdate=20 October 2013}}</ref> To date there has been no reported case of confirmed and medically treated black mamba bite in children.<ref name=Hilligan>{{cite journal|last=Hilligan|first=R|title=Black mamba bites. A report of 2 cases|journal=South African Medical Journal|date=1|year=1987|month=August|volume=72|issue=3|pages=220-1|pmid=3603321|url=http://www.ncbi.nlm.nih.gov/pubmed/3603321|accessdate=20 October 2013}}</ref> Coastal taipans can also be quite aggressive when cornered and will actively defend themselves.<ref name="DD"/> Untreated [[black mamba]] (''Dendroaspis polylepis'') and [[coastal taipan]] (''Oxyuranus scutellatus'') bites have a mortality rate of 100%.<ref name='Davidson'>{{cite web|url=http://drdavidson.ucsd.edu/portals/0/snake/dendroa3.htm|title=IMMEDIATE FIRST AID|last=Davidson|first=Terence|publisher=University of California, San Diego}}</ref><ref name="DD">{{cite web|url= http://drdavidson.ucsd.edu/Portals/0/snake/Oxyura~2.htm|title= IMMEDIATE FIRST AID for bites by Australian taipan or common taipan}}</ref> Black mamba and coastal taipan bites require very rapid and vigorous antivenom therapy as they are almost always fatal. The venoms of both species are exceptionally quick acting and both can cause human fatality in as little as 15-30 minutes. Black mambas in particular have been known to cause death in as little as 20 minutes post-envenomation.<ref name=NG/><ref name=NW/> These two snake species are generally accepted to be the deadliest snakes in the world by most herpetologists. |
||
===Other species=== |
===Other species=== |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
Other species that are of particular concern are the [[common krait]] (''Bungarus caeruleus''), which is often considered to be the most dangerous Asian snake species. It has a 70-80% mortality rate,<ref name="ct2">{{cite web|title=Clinical Toxinology-''Bungarus caeruleus''|url=http://toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0015|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:70-80%}}</ref> the [[inland taipan]] (''Oxyuranus microlepidotus'') which has a 80% mortality rate. The inland taipan is known to be a very shy, reclusive and a laid-back snake that will most always slither away from disturbance. It is not an aggressive species and rarely strikes.<ref>{{cite web|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0520|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:80%}}</ref> The [[Eastern brown snake]] (''Pseudonaja textilis''), which is the second most venomous land snake in the world based on {{LD50}} studies conducted on mice, is legendary for its bad temper, aggression, and for its speed. This species is responsible for more deaths every year in Australia than any other group of snakes.<ref name=AG>{{cite web|title=Australia's 10 most dangerous snakes|url=http://www.australiangeographic.com.au/journal/view-image.htm?gid=11893|work=Australian Geographic|publisher=Australian Geographic|accessdate=20 October 2013}}</ref> |
Other species that are of particular concern are the [[common krait]] (''Bungarus caeruleus''), which is often considered to be the most dangerous Asian snake species. It has a 70-80% mortality rate,<ref name="ct2">{{cite web|title=Clinical Toxinology-''Bungarus caeruleus''|url=http://toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0015|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:70-80%}}</ref> the [[inland taipan]] (''Oxyuranus microlepidotus'') which has a 80% mortality rate. The inland taipan is known to be a very shy, reclusive and a laid-back snake that will most always slither away from disturbance. It is not an aggressive species and rarely strikes.<ref>{{cite web|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0520|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:80%}}</ref> The [[Eastern brown snake]] (''Pseudonaja textilis''), which is the second most venomous land snake in the world based on {{LD50}} studies conducted on mice, is legendary for its bad temper, aggression, and for its speed. This species is responsible for more deaths every year in Australia than any other group of snakes.<ref name=AG>{{cite web|title=Australia's 10 most dangerous snakes|url=http://www.australiangeographic.com.au/journal/view-image.htm?gid=11893|work=Australian Geographic|publisher=Australian Geographic|accessdate=20 October 2013}}</ref> |
||
| ⚫ | |||
| ⚫ | The [[Saw-scaled viper]]s (''Echis carinatus'') are small, but their irritability, aggressive nature, and lethal venom potency make them very dangerous. These snakes are quick to strike, and mortality rates for those bitten are very high. In the regions where they occur, it is believed that saw-scaled vipers are responsible for more human deaths than all other snake species combined.<ref name=EB>{{cite web|title=Saw-scaled viper|url=http://www.britannica.com/EBchecked/topic/525886/saw-scaled-viper|work=Encyclopedia Britannica|publisher=Encyclopedia Britannica|accessdate=20 October 2013}}</ref> The rate of envenomation is over 80%.<ref name=Echis>{{cite web|title=Clinical Toxinology-''Echis carinatus'' caeruleus''|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0057|title= University of Adelaide Clinical Toxinology Resources}}</ref> The common death adder (''Acanthophis antarcticus'') is a highly venomous snake species with a 50-60% untreated mortality rate.<ref>{{cite web|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0491|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:50-60%}}</ref> Unlike other snakes that flee from approaching humans crashing through the undergrowth, common death adders are more likely to sit tight and risk being stepped on, making them more dangerous to the unwary bushwalker. They are said to be reluctant to bite unless actually touched.<ref name=DA>{{cite web|title=Australia's 10 most dangerous snakes|url=http://www.australiangeographic.com.au/journal/view-image.htm?index=8&gid=11893|work=Australian Geographic|publisher=Australian Geographic|accessdate=20 October 2013}}</ref> [[Tiger snake]]s (''genus Notechis'') are highly venomous. Their venoms possess potent [[neurotoxin]]s, [[Coagulation|coagulant]]s, [[haemolysin]]s and [[myotoxin]]s and the venom is quick-acting with rapid onset of breathing difficulties and paralysis. The untreated mortality rate from tiger snake bites is reported to be between 40 and 60%.<ref>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0540 University of Adelaide Clinical Toxinology Resource]</ref> The [[Gaboon viper]] (''Bitis gabonica''), although generally docile and sluggish, they have the longest fangs of any venomous snake and their venom glands are enormous and each bite produces the largest quantities of venom of any [[venomous snake]]. Yield is probably related to body weight, as opposed to milking interval.<ref name="Mal03">Mallow D, Ludwig D, Nilson G. 2003. ''True Vipers: Natural History and Toxinology of Old World Vipers''. Malabar, Florida: Krieger Publishing Company. 359 pp. ISBN 0-89464-877-2.</ref> Brown (1973) gives a venom yield range of 200–1000 mg (of dried venom),<ref name="Bro73">Brown JH. 1973. ''Toxicology and Pharmacology of Venoms from Poisonous Snakes''. Springfield, Illinois: Charles C. Thomas. 184 pp. LCCCN 73-229. ISBN 0-398-02808-7.</ref> A range of 200–600 mg for specimens 125–155 cm in length has also been reported.<ref name="Mal03"/> Spawls and Branch (1995) state from 5 to 7 ml (450–600 mg) of venom may be injected in a single bite.<ref name="SB95">Spawls S, [[William Roy Branch|Branch B]]. 1995. ''The Dangerous Snakes of Africa''. Ralph Curtis Books. Dubai: Oriental Press. 192 pp. ISBN 0-88359-029-8.</ref> A study by Marsh and Whaler (1984) reported a maximum yield of 9.7 ml of wet venom, which translated to 2400 mg of dried venom. They attached [[Crocodile clip|"alligator" clip electrodes]] to the angle of the open jaw of [[Anesthesia|anesthetized]] specimens (length 133–136 cm, girth 23–25 cm, weight 1.3–3.4 kg), yielding 1.3–7.6 ml (mean 4.4 ml) of venom. Two to three electrical bursts within a space of five seconds apart were enough to empty the venom glands. The snakes used for the study were milked seven to 11 times over a 12-month period, during which they remained in good health and the potency of their venom remained the same.<ref name="Mal03"/> |
||
| ⚫ | |||
| ⚫ | The [[Saw-scaled viper]]s (''Echis carinatus'') are small, but their irritability, aggressive nature, and lethal venom potency make them very dangerous. These snakes are quick to strike, and mortality rates for those bitten are very high. In the regions where they occur, it is believed that saw-scaled vipers are responsible for more human deaths than all other snake species combined.<ref name=EB>{{cite web|title=Saw-scaled viper|url=http://www.britannica.com/EBchecked/topic/525886/saw-scaled-viper|work=Encyclopedia Britannica|publisher=Encyclopedia Britannica|accessdate=20 October 2013}}</ref> The rate of envenomation is over 80%.<ref name=Echis>{{cite web|title=Clinical Toxinology-''Echis carinatus'' caeruleus''|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0057|title= University of Adelaide Clinical Toxinology Resources}}</ref> The common death adder (''Acanthophis antarcticus'') is a highly venomous snake species with a 50-60% untreated mortality rate.<ref>{{cite web|url=http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0491|title= University of Adelaide Clinical Toxinology Resources|quote=Mortality rate:50-60%}}</ref> Unlike other snakes that flee from approaching humans crashing through the undergrowth, common death adders are more likely to sit tight and risk being stepped on, making them more dangerous to the unwary bushwalker. They are said to be reluctant to bite unless actually touched.<ref name=DA>{{cite web|title=Australia's 10 most dangerous snakes|url=http://www.australiangeographic.com.au/journal/view-image.htm?index=8&gid=11893|work=Australian Geographic|publisher=Australian Geographic|accessdate=20 October 2013}}</ref> [[Tiger snake]]s (''genus Notechis'') are highly venomous. Their venoms possess potent [[neurotoxin]]s, [[Coagulation|coagulant]]s, [[haemolysin]]s and [[myotoxin]]s and the venom is quick-acting with rapid onset of breathing difficulties and paralysis. The untreated mortality rate from tiger snake bites is reported to be between 40 and 60%.<ref>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0540 University of Adelaide Clinical Toxinology Resource]</ref> |
||
Green mambas (Western, Eastern, and Jameson's) are all highly venomous snakes with bad tempers and a tendency to strike repeatedly with little provocation. The [[Western green mamba]] (''Dendroaspis viridis'') is highly venomous and aggressive with a {{LD50}} of 0.7 mg/kg [[Subcutaneous injection|SC]] and the average venom yield per bite is approximately 100 mg. The mortality rate of untreated bites is unknown but is thought to be very high (≫80%). The [[Eastern green mamba]] (''Dendroaspis angusticeps'') has an average venom yield per bite of 80 mg according to Engelmann and Obst (1981).<ref name=Engelmann>{{cite book|last=Engelmann|first=Wolf-Eberhard|title=Snakes: Biology, Behavior, and Relationship to Man|year=1981|publisher=Leipzig Publishing; English version published by Exeter Books (1982)|location=Leipzig; English version NY, USA|isbn=0-89673-110-3|pages=51}}</ref> The [[subcutaneous injection|subcutaneous]] {{LD50}} for this species ranges from 0.40 mg/kg to 3.05 mg/kg depending on different toxicology studies, authority figures and estimates. The mortality rate of untreated bites is unknown but is thought to be very high (75% +). The [[Jameson's mamba]] (''Dendroaspis jamesoni'') is known to be quite aggressive and defensive. The average venom yield per bite for this species is 80 mg, but some specimens may yield as much as 120 mg in a single bite. The [[Subcutaneous injection|SC]] {{LD50}} for this species according to Brown (1973) is 1.0 mg/kg, while the [[Intravenous therapy|IV]] {{LD50}} is 0.8 mg/kg.<ref name=Brown73>{{cite book|last=Brown|first=John H.|title=Toxicology and Pharmacology of Venoms from Poisonous Snakes|year=1973|publisher=Charles C. Thomas|location=Springfield, IL USA|isbn=0-398-02808-7|pages=81}}</ref> Envenomation by a Jameson's mamba can be deadly in as little as 30 to 120 minutes after being bitten, if proper medical treatment is not attained.<ref name='Davidson'>{{cite web|url=http://drdavidson.ucsd.edu/Portals/0/snake/Dendroa1.htm|title=IMMEDIATE FIRST AID|last=Davidson|first=Terence|publisher=University of California, San Diego}}</ref> The mortality rate of untreated bites is not exactly known, but it's said to be very high (≫ 80%).<ref name='WCH'>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0169 Clinical Toxinology Resource (''Dendroaspis jamesoni'')]</ref> |
Green mambas (Western, Eastern, and Jameson's) are all highly venomous snakes with bad tempers and a tendency to strike repeatedly with little provocation. The [[Western green mamba]] (''Dendroaspis viridis'') is highly venomous and aggressive with a {{LD50}} of 0.7 mg/kg [[Subcutaneous injection|SC]] and the average venom yield per bite is approximately 100 mg. The mortality rate of untreated bites is unknown but is thought to be very high (≫80%). The [[Eastern green mamba]] (''Dendroaspis angusticeps'') has an average venom yield per bite of 80 mg according to Engelmann and Obst (1981).<ref name=Engelmann>{{cite book|last=Engelmann|first=Wolf-Eberhard|title=Snakes: Biology, Behavior, and Relationship to Man|year=1981|publisher=Leipzig Publishing; English version published by Exeter Books (1982)|location=Leipzig; English version NY, USA|isbn=0-89673-110-3|pages=51}}</ref> The [[subcutaneous injection|subcutaneous]] {{LD50}} for this species ranges from 0.40 mg/kg to 3.05 mg/kg depending on different toxicology studies, authority figures and estimates. The mortality rate of untreated bites is unknown but is thought to be very high (75% +). The [[Jameson's mamba]] (''Dendroaspis jamesoni'') is known to be quite aggressive and defensive. The average venom yield per bite for this species is 80 mg, but some specimens may yield as much as 120 mg in a single bite. The [[Subcutaneous injection|SC]] {{LD50}} for this species according to Brown (1973) is 1.0 mg/kg, while the [[Intravenous therapy|IV]] {{LD50}} is 0.8 mg/kg.<ref name=Brown73>{{cite book|last=Brown|first=John H.|title=Toxicology and Pharmacology of Venoms from Poisonous Snakes|year=1973|publisher=Charles C. Thomas|location=Springfield, IL USA|isbn=0-398-02808-7|pages=81}}</ref> Envenomation by a Jameson's mamba can be deadly in as little as 30 to 120 minutes after being bitten, if proper medical treatment is not attained.<ref name='Davidson'>{{cite web|url=http://drdavidson.ucsd.edu/Portals/0/snake/Dendroa1.htm|title=IMMEDIATE FIRST AID|last=Davidson|first=Terence|publisher=University of California, San Diego}}</ref> The mortality rate of untreated bites is not exactly known, but it's said to be very high (≫ 80%).<ref name='WCH'>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0169 Clinical Toxinology Resource (''Dendroaspis jamesoni'')]</ref> |
||
| Line 158: | Line 151: | ||
Other than the Saw-scaled viper and the common krait, the species listed here are not as venomous as the species mentioned above, but they are known to cause a high amount of human fatalities annually. The most well known are the [[Big Four (Indian snakes)|Big Four]]. The Big Four are the four venomous snake species responsible for causing the most snake bite cases in South Asia (mostly in India). The Big Four snakes cause far more snakebites because they are much more abundant in highly-populated areas. They are the [[Indian cobra]] (''Naja naja''), [[common krait]] (''Bungarus caeruleus''), [[Russell's viper]] (''Daboia russelii'') and the [[Echis carinatus|Saw-scaled viper]] (''Echis carinatus'').<ref name="Whi90">Whitaker Z. 1990. Snakeman. Penguin Books Ltd. 192 pp. ISBN 0-14-014308-4.</ref> |
Other than the Saw-scaled viper and the common krait, the species listed here are not as venomous as the species mentioned above, but they are known to cause a high amount of human fatalities annually. The most well known are the [[Big Four (Indian snakes)|Big Four]]. The Big Four are the four venomous snake species responsible for causing the most snake bite cases in South Asia (mostly in India). The Big Four snakes cause far more snakebites because they are much more abundant in highly-populated areas. They are the [[Indian cobra]] (''Naja naja''), [[common krait]] (''Bungarus caeruleus''), [[Russell's viper]] (''Daboia russelii'') and the [[Echis carinatus|Saw-scaled viper]] (''Echis carinatus'').<ref name="Whi90">Whitaker Z. 1990. Snakeman. Penguin Books Ltd. 192 pp. ISBN 0-14-014308-4.</ref> |
||
==Gallery== |
|||
| ⚫ | |||
<gallery> |
|||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
File:Eastern Green Mamba 02.jpg|Eastern green mamba |
|||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
File:Dendroaspis viridisPCCA20051227-1885B.jpg|Western green mamba |
|||
File:GaboonViper2.jpg|Gaboon viper |
|||
File:Indiancobra.jpg|Indian cobra |
|||
</gallery> |
|||
| ⚫ | |||
[[King cobra]]s (''Ophiophagus hannah'') are not particularly venomous nor are they aggressive or bad tempered. Its venom toxicity is 1.80 mg/kg [[Subcutaneous injection|SC]] according to Broad et al. (1979).<ref name=tox>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0048 University of Adelaide Clinical Toxinology Resource]</ref> The mean value of subcutaneous {{LD50}} of five wild-caught king cobras in [[Southeast Asia]] was determined as 1.93 mg/kg.<ref name="CRC Press">{{cite book |title=Handbook of clinical toxicology of animal venoms and poisons|publisher=CRC Press|volume=236|year=1995|location=USA|isbn=0-8493-4489-1}}</ref> However, because the king cobra is the largest venomous snake in the world, it can inject very high amounts of venom in a victim. Between 350 to 500 mg (dry weight) of venom can be injected at once (Minton, 1974). In another study by (Broad et al, 1979), the average venom quantity was 421 mg (dry weight of milked venom).<ref name=tox/> The king cobra has a fearsome reputation. When annoyed, it spreads a narrow hood and growls loudly, but scientists claim that their "legendary aggressiveness" is grossly exaggerated.<ref name=Greene>{{cite book|last=Greene|first=HW|title=Snakes: The Evolution of Mystery in Nature|year=1997|publisher=University of California Press|location=California, USA|isbn=0520224876}}</ref> In most of the local encounters with live, wild king cobras, the snakes appear to be of rather placid disposition, and they usually end up being killed or subdued with hardly any hysterics. These support the view that wild king cobras generally have a mild temperament, and despite their frequent occurrence in disturbed and built-up areas, are adept at avoiding humans. Naturalist Michael Wilmer Forbes Tweedie felt that "this notion is based on the general tendency to dramatise all attributes of snakes with little regard for the truth about them. A moment’s reflection shows that this must be so, for the species is not uncommon, even in populated areas, and consciously or unconsciously, people must encounter king cobras quite frequently. If the snake were really habitually aggressive records of its bite would be frequent; as it is they are extremely rare."<ref name=Tweedie>{{cite book|last=Tweedie|first=MWF|title=The Snakes of Malaya|year=1983|publisher=Singapore National Printers Ltd|location=Singapore|isbn=B0007B41IO}}</ref> Mortality rates vary sharply depending on many factors. Most bites involve non-fatal amounts.<ref name=MG>{{cite web|last=Mathew, Gera|first=JL, T|title=http://www.priory.com/med/ophitoxaemia.htm|url=http://www.priory.com/med/ophitoxaemia.htm|work=MEDICINE ON-LINE|accessdate=20 October 2013}}</ref> |
[[King cobra]]s (''Ophiophagus hannah'') are not particularly venomous nor are they aggressive or bad tempered. Its venom toxicity is 1.80 mg/kg [[Subcutaneous injection|SC]] according to Broad et al. (1979).<ref name=tox>[http://www.toxinology.com/fusebox.cfm?fuseaction=main.snakes.display&id=SN0048 University of Adelaide Clinical Toxinology Resource]</ref> The mean value of subcutaneous {{LD50}} of five wild-caught king cobras in [[Southeast Asia]] was determined as 1.93 mg/kg.<ref name="CRC Press">{{cite book |title=Handbook of clinical toxicology of animal venoms and poisons|publisher=CRC Press|volume=236|year=1995|location=USA|isbn=0-8493-4489-1}}</ref> However, because the king cobra is the largest venomous snake in the world, it can inject very high amounts of venom in a victim. Between 350 to 500 mg (dry weight) of venom can be injected at once (Minton, 1974). In another study by (Broad et al, 1979), the average venom quantity was 421 mg (dry weight of milked venom).<ref name=tox/> The king cobra has a fearsome reputation. When annoyed, it spreads a narrow hood and growls loudly, but scientists claim that their "legendary aggressiveness" is grossly exaggerated.<ref name=Greene>{{cite book|last=Greene|first=HW|title=Snakes: The Evolution of Mystery in Nature|year=1997|publisher=University of California Press|location=California, USA|isbn=0520224876}}</ref> In most of the local encounters with live, wild king cobras, the snakes appear to be of rather placid disposition, and they usually end up being killed or subdued with hardly any hysterics. These support the view that wild king cobras generally have a mild temperament, and despite their frequent occurrence in disturbed and built-up areas, are adept at avoiding humans. Naturalist Michael Wilmer Forbes Tweedie felt that "this notion is based on the general tendency to dramatise all attributes of snakes with little regard for the truth about them. A moment’s reflection shows that this must be so, for the species is not uncommon, even in populated areas, and consciously or unconsciously, people must encounter king cobras quite frequently. If the snake were really habitually aggressive records of its bite would be frequent; as it is they are extremely rare."<ref name=Tweedie>{{cite book|last=Tweedie|first=MWF|title=The Snakes of Malaya|year=1983|publisher=Singapore National Printers Ltd|location=Singapore|isbn=B0007B41IO}}</ref> Mortality rates vary sharply depending on many factors. Most bites involve non-fatal amounts.<ref name=MG>{{cite web|last=Mathew, Gera|first=JL, T|title=http://www.priory.com/med/ophitoxaemia.htm|url=http://www.priory.com/med/ophitoxaemia.htm|work=MEDICINE ON-LINE|accessdate=20 October 2013}}</ref> |
||
Revision as of 00:04, 21 October 2013
| Snakebite | |
|---|---|
| Specialty | Emergency medicine |
A snakebite is an injury caused by a bite from a snake, often resulting in puncture wounds inflicted by the animal's fangs and sometimes resulting in envenomation. Although the majority of snake species are non-venomous and typically kill their prey with constriction rather than venom, venomous snakes can be found on every continent except Antarctica.[1] Snakes often bite their prey as a method of hunting, but also for defensive purposes against predators. Since the physical appearance of snakes may differ, there is often no practical way to identify a species and professional medical attention should be sought.[2][3]
The outcome of snake bites depends on numerous factors, including the species of snake, the area of the body bitten, the amount of venom injected, and the health conditions of the person. Feelings of terror and panic are common after a snakebite and can produce a characteristic set of symptoms mediated by the autonomic nervous system, such as a racing heart and nausea.[4][5] Bites from non-venomous snakes can also cause injury, often due to lacerations caused by the snake's teeth, or from a resulting infection. A bite may also trigger an anaphylactic reaction, which is potentially fatal. First aid recommendations for bites depend on the snakes inhabiting the region, as effective treatments for bites inflicted by some species can be ineffective for others.
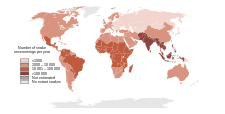
The number of fatalities attributed to snake bites varies greatly by geographical area. Although deaths are relatively rare in Australia, Europe and North America,[1][6][7] the morbidity and mortality associated with snake bites is a serious public health problem in many regions of the world, particularly in rural areas lacking medical facilities. Further, while South Asia, Southeast Asia, and sub-Saharan Africa report the highest number of bites, there is also a high incidence in the Neotropics and other equatorial and subtropical regions.[1][6][7] Each year tens of thousands of people die from snake bites,[1] yet the risk of being bitten can be lowered with preventive measures, such as wearing protective footwear and avoiding areas known to be inhabited by dangerous snakes.
Signs and symptoms

The most common symptoms of all snakebites are overwhelming fear, panic, and emotional instability, which may cause symptoms such as nausea and vomiting, diarrhea, vertigo, fainting, tachycardia, and cold, clammy skin.[4][5] Television, literature, and folklore are in part responsible for the hype surrounding snakebites, and people may have unwarranted thoughts of imminent death.
Dry snakebites, and those inflicted by a non-venomous species, can still cause severe injury. There are several reasons for this: a snakebite may become infected with the snake's saliva and fangs sometimes harboring pathogenic microbial organisms, including Clostridium tetani. Infection is often reported with viper bites whose fangs are capable of deep puncture wounds. Bites may cause anaphylaxis in certain people.
Most snakebites, whether by a venomous snake or not, will have some type of local effect. There is minor pain and redness in over 90% of cases, although this varies depending on the site.[4] Bites by vipers and some cobras may be extremely painful, with the local tissue sometimes becoming tender and severely swollen within 5 minutes.[7] This area may also bleed and blister and can eventually lead to tissue necrosis. Other common initial symptoms of pitviper and viper bites include lethargy, bleeding, weakness, nausea, and vomiting.[4][7] Symptoms may become more life-threatening over time, developing into hypotension, tachypnea, severe tachycardia, severe internal bleeding, altered sensorium, kidney failure, and respiratory failure.[4][7]
Interestingly, bites caused by the Mojave rattlesnake, kraits, coral snake, and the speckled rattlesnake reportedly cause little or no pain despite being serious injuries.[4] Those bitten may also describe a "rubbery," "minty," or "metallic" taste if bitten by certain species of rattlesnake.[4] Spitting cobras and rinkhalses can spit venom in a persons eyes. This results in immediate pain, ophthalmoparesis, and sometimes blindness.[11][12]

Some Australian elapids and most viper envenomations will cause coagulopathy, sometimes so severe that a person may bleed spontaneously from the mouth, nose, and even old, seemingly-healed wounds.[7] Internal organs may bleed, including the brain and intestines and will cause ecchymosis (bruising) of the skin.
Venom emitted from elapids, including sea snakes, kraits, cobras, king cobra, mambas, and many Australian species, contain toxins which attack the nervous system, causing neurotoxicity.[4][7][14] The person may present with strange disturbances to their vision, including blurriness. Paresthesia throughout the body, as well as difficulty in speaking and breathing, may be reported.[4] Nervous system problems will cause a huge array of symptoms, and those provided here are not exhaustive. If not treated immediately they may die from respiratory failure.
Venom emitted from some types of cobras, almost all vipers, some Australian elapids and some sea snakes causes necrosis of muscle tissue.[7] Muscle tissue will begin to die throughout the body, a condition known as rhabdomyolysis. Rhabdomyolysis can result in damage to the kidneys as a result of myoglobin accumulation in the renal tubules. This, coupled with hypotension, can lead to acute renal failure, and, if left untreated, eventually death.[7]
Pathophysiology
Since envenomation is completely voluntary, all venomous snakes are capable of biting without injecting venom into a person. Snakes may deliver such a "dry bite" rather than waste their venom on a creature too large for them to eat, a behavour called venom metering.[15] However, the percentage of dry bites varies between species: 80% of bites inflicted by sea snakes, which are normally timid, do not result in envenomation,[14] whereas only 25% of pitviper bites are dry.[4] Furthermore, some snake genera, such as rattlesnakes, significantly increase the amount of venom injected in defensive bites compared to predatory strikes.[16]
Some dry bites may also be the result of imprecise timing on the snake's part, as venom may be prematurely released before the fangs have penetrated the person.[15] Even without venom, some snakes, particularly large constrictors such as those belonging to the Boidae and Pythonidae families, can deliver damaging bites; large specimens often cause severe lacerations, or the snake itself pulls away, causing the flesh to be torn by the needle-sharp recurved teeth embedded in the person. While not as life-threatening as a bite from a venomous species, the bite can be at least temporarily debilitating and could lead to dangerous infections if improperly dealt with.
While most snakes must open their mouths before biting, African and Middle Eastern snakes belonging to the family Atractaspididae are able to fold their fangs to the side of their head without opening their mouth and jab a person.[17]
Snake venom
It has been suggested that snakes evolved the mechanisms necessary for venom formation and delivery sometime during the Miocene epoch.[18] During the mid-Tertiary, most snakes were large ambush predators belonging to the superfamily Henophidia, which use constriction to kill their prey. As open grasslands replaced forested areas in parts of the world, some snake families evolved to become smaller and thus more agile. However, subduing and killing prey became more difficult for the smaller snakes, leading to the evolution of snake venom.[18] Other research on Toxicofera, a hypothetical clade thought to be ancestral to most living reptiles, suggests an earlier time frame for the evolution of snake venom, possibly to the order of tens of millions of years, during the Late Cretaceous.[19]
Snake venom is produced in modified parotid glands normally responsible for secreting saliva. It is stored in structures called alveoli behind the animal's eyes, and ejected voluntarily through its hollow tubular fangs. Venom is composed of hundreds to thousands of different proteins and enzymes, all serving a variety of purposes, such as interfering with a prey's cardiac system or increasing tissue permeability so that venom is absorbed faster.
Venom in many snakes, such as pitvipers, affects virtually every organ system in the human body and can be a combination of many toxins, including cytotoxins, hemotoxins, neurotoxins, and myotoxins, allowing for an enormous variety of symptoms.[4][20] Earlier, the venom of a particular snake was considered to be one kind only i.e. either hemotoxic or neurotoxic, and this erroneous belief may still persist wherever the updated literature is hard to access. Although there is much known about the protein compositions of venoms from Asian and American snakes, comparatively little is known of Australian snakes.
The strength of venom differs markedly between species and even more so between families, as measured by median lethal dose (LD50) in mice. Subcutaneous LD50 varies by over 140-fold within elapids and by more than 100-fold in vipers. The amount of venom produced also differs among species, with the Gaboon viper able to potentially deliver from 450–600 milligrams of venom in a single bite, the most of any snake.[21] Opisthoglyphous colubrids have venom ranging from life-threatening (in the case of the boomslang) to barely noticeable (as in Tantilla).
Prevention

Snakes are most likely to bite when they feel threatened, are startled, are provoked, or have no means of escape when cornered. Encountering a snake is potentially dangerous and it is recommended to leave the vicinity. It is difficult to safely identify many snake species as appearances may vary dramatically.
Snakes are likely to approach residential areas when attracted by prey, such as rodents. Practising regular pest control can reduce the threat of snakes considerably. It is beneficial to know the species of snake that are common in local areas, or while travelling or hiking. Areas of the world such as Africa, Australia, the Neotropics, and southern Asia are inhabited by many highly dangerous species. Being wary of snake presence and ultimately avoiding it when known is strongly recommended.
When in the wilderness, treading heavily creates ground vibrations and noise, which will often cause snakes to flee from the area. However, this generally only applies to North America as some larger and more aggressive snakes in other parts of the world, such as king cobras[22] and black mambas,[23] will protect their territories. When dealing with direct encounters it is best to remain silent and motionless. If the snake has not yet fled it is important to step away slowly and cautiously.
The use of a flashlight when engaged in camping activities, such as gathering firewood at night, can be helpful. Snakes may also be unusually active during especially warm nights when ambient temperatures exceed 21 °C (70 °F). It is advised not to reach blindly into hollow logs, flip over large rocks, and enter old cabins or other potential snake hiding-places. When rock climbing, it is not safe to grab ledges or crevices without examining them first, as snakes are cold-blooded and often sunbathe atop rock ledges.
In the United States more than 40% of people bitten by snake intentionally put themselves in harm's way by attempting to capture wild snakes or by carelessly handling their dangerous pets—40% of that number had a blood alcohol level of 0.1% or more.[24]
It is also important to avoid snakes that appear to be dead, as some species will actually roll over on their backs and stick out their tongue to fool potential threats. A snake's detached head can immediately act by reflex and potentially bite. The induced bite can be just as severe as that of a live snake.[4][25] Dead snakes are also incapable of regulating the venom they inject, so a bite from a dead snake can often contain large amounts of venom.[26]
Treatment
It is not an easy task determining whether or not a bite by any species of snake is life-threatening. A bite by a North American copperhead on the ankle is usually a moderate injury to a healthy adult, but a bite to a child's abdomen or face by the same snake may be fatal. The outcome of all snakebites depends on a multitude of factors: the size, physical condition, and temperature of the snake, the age and physical condition of the person, the area and tissue bitten (e.g., foot, torso, vein or muscle), the amount of venom injected, the time it takes for the person to find treatment, and finally the quality of that treatment.[4][27]
Snake identification
Identification of the snake is important in planning treatment in certain areas of the world, but is not always possible. Ideally the dead snake would be brought in with the person, but in areas where snake bite is more common, local knowledge may be sufficient to recognize the snake. However, in regions where polyvalent antivenoms are available, such as North America, identification of snake is not a high priority item. Attempting to catch or kill the offending snake also puts one at risk for re-envenomation or creating a second person bitten, and generally is not recommended.
The three types of venomous snakes that cause the majority of major clinical problems are vipers, kraits, and cobras. Knowledge of what species are present locally can be crucial, as is knowledge of typical signs and symptoms of envenomation by each type of snake. A scoring system can be used to try to determine the biting snake based on clinical features,[28] but these scoring systems are extremely specific to particular geographical areas.
First aid
Snakebite first aid recommendations vary, in part because different snakes have different types of venom. Some have little local effect, but life-threatening systemic effects, in which case containing the venom in the region of the bite by pressure immobilization is desirable. Other venoms instigate localized tissue damage around the bitten area, and immobilization may increase the severity of the damage in this area, but also reduce the total area affected; whether this trade-off is desirable remains a point of controversy. Because snakes vary from one country to another, first aid methods also vary.
However, most first aid guidelines agree on the following:
- Protect the person and others from further bites. While identifying the species is desirable in certain regions, risking further bites or delaying proper medical treatment by attempting to capture or kill the snake is not recommended.
- Keep the person calm. Acute stress reaction increases blood flow and endangers the person. Panic is infectious and compromises judgment.
- Call for help to arrange for transport to the nearest hospital emergency room, where antivenom for snakes common to the area will often be available.
- Make sure to keep the bitten limb in a functional position and below the person's heart level so as to minimize blood returning to the heart and other organs of the body.
- Do not give the person anything to eat or drink. This is especially important with consumable alcohol, a known vasodilator which will speed up the absorption of venom. Do not administer stimulants or pain medications, unless specifically directed to do so by a physician.
- Remove any items or clothing which may constrict the bitten limb if it swells (rings, bracelets, watches, footwear, etc.)
- Keep the person as still as possible.
- Do not incise the bitten site.
Many organizations, including the American Medical Association and American Red Cross, recommend washing the bite with soap and water. Australian recommendations for snake bite treatment recommend against cleaning the wound. Traces of venom left on the skin/bandages from the strike can be used in combination with a snake bite identification kit to identify the species of snake. This speeds determination of which antivenom to administer in the emergency room.[29]
India developed a national snake-bite protocol in 2007 which includes advice to:[30]
- Reassure the patient. 70% of all snakebites are from non- venomous species. Only 50% of bites by venomous species actually envenomate the patient
- Immobilise in the same way as a fractured limb. Use bandages or cloth to hold the splints, not to block the blood supply or apply pressure. Do not apply any compression in the form of tight ligatures, they don’t work and can be dangerous!
- Get to Hospital Immediately. Traditional remedies have no proven benefit in treating snakebite.
- Tell the doctor of any systemic symptoms, such as droopiness of a body part, that manifest on the way to hospital.
Pressure immobilization
As of 2008, clinical evidence for pressure immobilization via the use of an elastic bandage is limited.[31] It is recommended for snakebite that have occurred in Australia (due to elapids which are neurotoxic).[32] It is not recommended for bites from non neurotoxic snakes such as found in North America and other regions of the world.[32][33] The British military recommends pressure immobilization in all cases where the type of snake is unknown.[34]
The object of pressure immobilization is to contain venom within a bitten limb and prevent it from moving through the lymphatic system to the vital organs. This therapy has two components: pressure to prevent lymphatic drainage, and immobilization of the bitten limb to prevent the pumping action of the skeletal muscles.
Antivenom
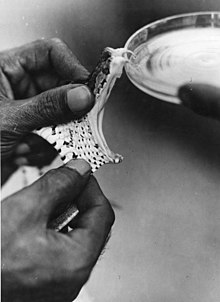
Until the advent of antivenom, bites from some species of snake were almost universally fatal.[35] Despite huge advances in emergency therapy, antivenom is often still the only effective treatment for envenomation. The first antivenom was developed in 1895 by French physician Albert Calmette for the treatment of Indian cobra bites. Antivenom is made by injecting a small amount of venom into an animal (usually a horse or sheep) to initiate an immune system response. The resulting antibodies are then harvested from the animal's blood.
Antivenom is injected into the person intravenously, and works by binding to and neutralizing venom enzymes. It cannot undo damage already caused by venom, so antivenom treatment should be sought as soon as possible. Modern antivenoms are usually polyvalent, making them effective against the venom of numerous snake species. Pharmaceutical companies which produce antivenom target their products against the species native to a particular area. Although some people may develop serious adverse reactions to antivenom, such as anaphylaxis, in emergency situations this is usually treatable and hence the benefit outweighs the potential consequences of not using antivenom.
Outmoded

The following treatments while once recommended are considered of no use or harmful including: tourniquets, incisions, suction, application of cold, and application of electricity.[33] Cases in which these treatments appear to work may be the result of dry bites.
- Application of a tourniquet to the bitten limb is generally not recommended. There is no convincing evidence that it is an effective first aid tool as ordinarily applied.[36] Tourniquets have been found to be completely ineffective in the treatment of Crotalus durissus bites,[37] but some positive results have been seen with properly applied tourniquets for cobra venom in the Philippines.[38] Uninformed tourniquet use is dangerous, since reducing or cutting off circulation can lead to gangrene, which can be fatal.[36] The use of a compression bandage is generally as effective, and much safer.
- Cutting open the bitten area, an action often taken prior to suction, is not recommended since it causes further damage and increases the risk of infection.
- Sucking out venom, either by mouth or with a pump, does not work and may harm the affected area directly.[39] Suction started after 3 minutes removes a clinically insignificant quantity—less than one thousandth of the venom injected—as shown in a human study.[40] In a study with pigs, suction not only caused no improvement but led to necrosis in the suctioned area.[41] Suctioning by mouth presents a risk of further poisoning through the mouth's mucous tissues.[42] The well-meaning family member or friend may also release bacteria into the persons wound, leading to infection.
- Immersion in warm water or sour milk, followed by the application of snake-stones (also known as la Pierre Noire), which are believed to draw off the poison in much the way a sponge soaks up water.
- Application of potassium permanganate.
- Use of electroshock therapy in animal tests has shown this treatment to be useless and potentially dangerous.[43][44][45][46]
In extreme cases, in remote areas, all of these misguided attempts at treatment have resulted in injuries far worse than an otherwise mild to moderate snakebite. In worst case scenarios, thoroughly constricting tourniquets have been applied to bitten limbs, completely shutting off blood flow to the area. By the time the person finally reached appropriate medical facilities their limbs had to be amputated.
Epidemiology
Most snakebites are caused by non-venomous snakes. Of the roughly 3,000 known species of snake found worldwide, only 15% are considered dangerous to humans.[1][4][47] Snakes are found on every continent except Antarctica.[1] The most diverse and widely distributed snake family, the colubrids, has approximately 700 venomous species,[48] but only five genera—boomslangs, twig snakes, keelback snakes, green snakes, and slender snakes—have caused human fatalities.[48]
Since reporting is not mandatory in many regions of the world,[1] snakebites often go unreported. Consequently, no accurate study has ever been conducted to determine the frequency of snakebites on the international level. However, some estimates put the number at 5.4 million snakebites, 2.5 million envenomings, resulting in perhaps 125,000 deaths.[1] Others estimate 1.2 to 5.5 million snakebites, 421,000 to 1.8 million envenomings, and 20,000 to 94,000 deaths.[1] Many people who survive bites nevertheless suffer from permanent tissue damage caused by venom, leading to disability.[7] Most snake envenomings and fatalities occur in South Asia, Southeast Asia, and sub-Saharan Africa, with India reporting the most snakebite deaths of any country.[1]
Worldwide, snakebites occur most frequently in the summer season when snakes are active and humans are outdoors.[1][49] Agricultural and tropical regions report more snakebites than anywhere else.[1][50] In the USA, those bitten are typically male and between 17 and 27 years of age.[4][49][51] Children and the elderly are the most likely to die.[4][27]
Snakes of particular concern
Black mamba and Coastal taipan


Clinical mortality rate (often determined by measured toxicity on mice) is a commonly used indicator to determine the danger of any given venomous snake, but important too are its efficiency of venom delivery, its venom yield and its behavior when it encounters humans. Black mambas in particular are known to be high-strung, are the fastest snake species in the world, are highly aggressive, defensive and they are well known to have an irascible temperament.[22][52] Black mambas are also known to be the most accurate strikers, usually striking several times in quick succession. They are also known to have a 100% rate of envenomation. The probability of dry bites (no venom injected) in black mamba strikes is almost non-existent.[53][54] To date there has been no reported case of confirmed and medically treated black mamba bite in children.[55] Coastal taipans can also be quite aggressive when cornered and will actively defend themselves.[56] Untreated black mamba (Dendroaspis polylepis) and coastal taipan (Oxyuranus scutellatus) bites have a mortality rate of 100%.[53][56] Black mamba and coastal taipan bites require very rapid and vigorous antivenom therapy as they are almost always fatal. The venoms of both species are exceptionally quick acting and both can cause human fatality in as little as 15-30 minutes. Black mambas in particular have been known to cause death in as little as 20 minutes post-envenomation.[22][52] These two snake species are generally accepted to be the deadliest snakes in the world by most herpetologists.
Other species
Other species that are of particular concern are the common krait (Bungarus caeruleus), which is often considered to be the most dangerous Asian snake species. It has a 70-80% mortality rate,[57] the inland taipan (Oxyuranus microlepidotus) which has a 80% mortality rate. The inland taipan is known to be a very shy, reclusive and a laid-back snake that will most always slither away from disturbance. It is not an aggressive species and rarely strikes.[58] The Eastern brown snake (Pseudonaja textilis), which is the second most venomous land snake in the world based on LD50 studies conducted on mice, is legendary for its bad temper, aggression, and for its speed. This species is responsible for more deaths every year in Australia than any other group of snakes.[59]
The Saw-scaled vipers (Echis carinatus) are small, but their irritability, aggressive nature, and lethal venom potency make them very dangerous. These snakes are quick to strike, and mortality rates for those bitten are very high. In the regions where they occur, it is believed that saw-scaled vipers are responsible for more human deaths than all other snake species combined.[60] The rate of envenomation is over 80%.[61] The common death adder (Acanthophis antarcticus) is a highly venomous snake species with a 50-60% untreated mortality rate.[62] Unlike other snakes that flee from approaching humans crashing through the undergrowth, common death adders are more likely to sit tight and risk being stepped on, making them more dangerous to the unwary bushwalker. They are said to be reluctant to bite unless actually touched.[63] Tiger snakes (genus Notechis) are highly venomous. Their venoms possess potent neurotoxins, coagulants, haemolysins and myotoxins and the venom is quick-acting with rapid onset of breathing difficulties and paralysis. The untreated mortality rate from tiger snake bites is reported to be between 40 and 60%.[64] The Gaboon viper (Bitis gabonica), although generally docile and sluggish, they have the longest fangs of any venomous snake and their venom glands are enormous and each bite produces the largest quantities of venom of any venomous snake. Yield is probably related to body weight, as opposed to milking interval.[65] Brown (1973) gives a venom yield range of 200–1000 mg (of dried venom),[66] A range of 200–600 mg for specimens 125–155 cm in length has also been reported.[65] Spawls and Branch (1995) state from 5 to 7 ml (450–600 mg) of venom may be injected in a single bite.[67] A study by Marsh and Whaler (1984) reported a maximum yield of 9.7 ml of wet venom, which translated to 2400 mg of dried venom. They attached "alligator" clip electrodes to the angle of the open jaw of anesthetized specimens (length 133–136 cm, girth 23–25 cm, weight 1.3–3.4 kg), yielding 1.3–7.6 ml (mean 4.4 ml) of venom. Two to three electrical bursts within a space of five seconds apart were enough to empty the venom glands. The snakes used for the study were milked seven to 11 times over a 12-month period, during which they remained in good health and the potency of their venom remained the same.[65]
Green mambas (Western, Eastern, and Jameson's) are all highly venomous snakes with bad tempers and a tendency to strike repeatedly with little provocation. The Western green mamba (Dendroaspis viridis) is highly venomous and aggressive with a LD50 of 0.7 mg/kg SC and the average venom yield per bite is approximately 100 mg. The mortality rate of untreated bites is unknown but is thought to be very high (≫80%). The Eastern green mamba (Dendroaspis angusticeps) has an average venom yield per bite of 80 mg according to Engelmann and Obst (1981).[68] The subcutaneous LD50 for this species ranges from 0.40 mg/kg to 3.05 mg/kg depending on different toxicology studies, authority figures and estimates. The mortality rate of untreated bites is unknown but is thought to be very high (75% +). The Jameson's mamba (Dendroaspis jamesoni) is known to be quite aggressive and defensive. The average venom yield per bite for this species is 80 mg, but some specimens may yield as much as 120 mg in a single bite. The SC LD50 for this species according to Brown (1973) is 1.0 mg/kg, while the IV LD50 is 0.8 mg/kg.[69] Envenomation by a Jameson's mamba can be deadly in as little as 30 to 120 minutes after being bitten, if proper medical treatment is not attained.[53] The mortality rate of untreated bites is not exactly known, but it's said to be very high (≫ 80%).[70]
Other than the Saw-scaled viper and the common krait, the species listed here are not as venomous as the species mentioned above, but they are known to cause a high amount of human fatalities annually. The most well known are the Big Four. The Big Four are the four venomous snake species responsible for causing the most snake bite cases in South Asia (mostly in India). The Big Four snakes cause far more snakebites because they are much more abundant in highly-populated areas. They are the Indian cobra (Naja naja), common krait (Bungarus caeruleus), Russell's viper (Daboia russelii) and the Saw-scaled viper (Echis carinatus).[71]
Gallery
-
Common krait
-
Common death adder
-
Inland taipan
-
Eastern brown snake
-
Eastern green mamba
-
Saw-scaled viper
-
Jameson's mamba
-
Russell's viper
-
Tiger snake
-
Western green mamba
-
Gaboon viper
-
Indian cobra
Snakes with exaggerated temperaments and venom toxicity
King cobras (Ophiophagus hannah) are not particularly venomous nor are they aggressive or bad tempered. Its venom toxicity is 1.80 mg/kg SC according to Broad et al. (1979).[72] The mean value of subcutaneous LD50 of five wild-caught king cobras in Southeast Asia was determined as 1.93 mg/kg.[73] However, because the king cobra is the largest venomous snake in the world, it can inject very high amounts of venom in a victim. Between 350 to 500 mg (dry weight) of venom can be injected at once (Minton, 1974). In another study by (Broad et al, 1979), the average venom quantity was 421 mg (dry weight of milked venom).[72] The king cobra has a fearsome reputation. When annoyed, it spreads a narrow hood and growls loudly, but scientists claim that their "legendary aggressiveness" is grossly exaggerated.[74] In most of the local encounters with live, wild king cobras, the snakes appear to be of rather placid disposition, and they usually end up being killed or subdued with hardly any hysterics. These support the view that wild king cobras generally have a mild temperament, and despite their frequent occurrence in disturbed and built-up areas, are adept at avoiding humans. Naturalist Michael Wilmer Forbes Tweedie felt that "this notion is based on the general tendency to dramatise all attributes of snakes with little regard for the truth about them. A moment’s reflection shows that this must be so, for the species is not uncommon, even in populated areas, and consciously or unconsciously, people must encounter king cobras quite frequently. If the snake were really habitually aggressive records of its bite would be frequent; as it is they are extremely rare."[75] Mortality rates vary sharply depending on many factors. Most bites involve non-fatal amounts.[76]
The Boomslang (Dispholidus typus) is a rear-fanged venomous colubrid snake. It has a relatively high potency venom ranging from 0.06 - 0.72 mg/kg. This is sufficient to kill mice in 50% of cases, if the venom reaches a vein (LD50).[77] However, boomslangs are timid snakes, and bites generally occur only when people attempt to handle, catch or kill the animal. When confronted and cornered, they inflate their necks and assume their striking "S"-shaped pose. The above data suggest boomslangs are unlikely to be a significant source of human fatalities throughout their distribution range. In 1957, well-known herpetologist Karl Schmidt died after being bitten by a boomslang. D.S. Chapman stated eight serious human envenomations by boomslangs occurred between 1919 and 1962, two of which were fatal. The venom of this species is very slow to act, symptoms may not be manifested until many hours after the bite. While this provides time for procuring the antivenom, it also may lead victims to underestimate the seriousness of the bite. Boomslangs may sometimes fail to inject venom when they bite, so that even after a bite envenomation is not guaranteed.
Rattlesnakes (Crotalus) such as the Eastern diamondback rattlesnake (Crotalus adamanteus) and the Western diamondback rattlesnake (Crotalus atrox) are the leading causes of snakebite incidents in the United States, but they have a low venom potency and are generally not aggressive or combative. The western diamondback rattlesnake has LD50 values of 2.72 mg/kg IV, 20 mg/kg IM and 18.5 mg/kg SC, which is far less toxic than many other snakes and other rattlesnakes. Brown gives the eastern diamondback rattlesnake an average venom yield of 410 mg (dried venom), along with LD50 values of 1.3-2.4 mg/kg IV, 1.7-3.0 mg/kg IP and 14.5–10 mg/kg SC for toxicity, again much less venomous than most snakes.[66] With the exception of the Tiger rattlesnake (Crotalus tigris), the Neotropical rattlesnake (Crotalus durissus) and the Mojave rattlesnake (Crotalus scutulatus), most rattlesnakes are not a serious threat to human life. Bites are easily treatable and mortality rates are very low (≪ 10%).
Society and culture

Snakes were both revered and worshipped and feared by early civilizations. The ancient Egyptians recorded prescribed treatments for snakebites as early as the Thirteenth dynasty in the Brooklyn Papyrus, which includes at least seven venomous species common to the region today, such as the horned vipers.[78] In Judaism, the Nehushtan was a pole with a snake made of copper wrapped around it, similar in appearance to the Rod of Asclepius. The object was considered sacred with the power to heal bites caused by the snakes which had infested the desert, with people merely having to touch it in order to save themselves from imminent death.
Historically, snakebites were seen as a means of execution in some cultures. In medieval Europe, a form of capital punishment was to throw people into snake pits, leaving people to die from multiple venomous bites. A similar form of punishment was common in Southern Han during China's Five Dynasties and Ten Kingdoms period and in India.[79] Snakebites were also used as a form of suicide, most notably by Egyptian queen Cleopatra VII, who reportedly died from the bite of an asp—likely an Egyptian cobra[78][80]—after hearing of Mark Antony's death.
Snakebite as a surreptitious form of murder has been featured in stories such as Sir Arthur Conan Doyle's The Adventure of the Speckled Band, but actual occurrences are virtually unheard of, with only a few documented cases.[79][81][82] It has been suggested that Boris III of Bulgaria, who was allied to Nazi Germany during World War II, may have been killed with snake venom,[79] although there is no definitive evidence. At least one attempted suicide by snakebite has been documented in medical literature involving a puff adder bite to the hand.[83]
References
- ^ a b c d e f g h i j k l Kasturiratne, A.; Wickremasinghe A. R.; de Silva N.; Gunawardena N. K.; et al. (2008). Winkel, Ken (ed.). "The Global Burden of Snakebite: A Literature Analysis and Modelling Based on Regional Estimates of Envenoming and Deaths". PloS Medicine. 5 (11): e218. doi:10.1371/journal.pmed.0050218. PMC 2577696. PMID 18986210. Retrieved 2009-06-24.
{{cite journal}}: Unknown parameter|author-separator=ignored (help)CS1 maint: unflagged free DOI (link) - ^ "Snake Venom Detection Kit: Detection and Identification of Snake Venom" (PDF). CSL Limited. 2007. Retrieved 2009-11-24.
The physical identification of Australian and Papua New Guinean snakes is notoriously unreliable. There is often marked colour variation between juvenile and adult snakes and wide size, shape and colour variation between snakes of the same species. Reliable snake identification requires expert knowledge of snake anatomy, a snake key and the physical handling of the snake
{{cite journal}}: Cite journal requires|journal=(help) - ^ White, Julian (2006). "Snakebite & Spiderbite: Management Guidelines". Adelaide: Department of Health, Government of South Australia: 1–71. ISBN 0-7308-9551-3. Retrieved 2009-11-24.
The colour of brown snakes is very variable and misleading for identification purposes. They may be brown, red brown, grey, very dark brown and may be plain in color, have speckling, stripes or bands, or have a dark or black head
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b c d e f g h i j k l m n o p Gold, Barry S. (1 April 2002). "Bites of venomous snakes". The New England Journal of Medicine. 347 (5): 347–56. doi:10.1056/NEJMra013477. PMID 12151473.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Kitchens C, Van Mierop L (1987). "Envenomation by the Eastern coral snake (Micrurus fulvius fulvius). A study of 39 victims". JAMA. 258 (12): 1615–18. doi:10.1001/jama.258.12.1615. PMID 3625968.
- ^ a b Chippaux, J.P. (1998). "Snake-bites: appraisal of the global situation" (PDF). Bulletin of the World Health Organization. 76 (5): 515–24. PMC 2305789. PMID 9868843. Retrieved 2009-07-03.
- ^ a b c d e f g h i j Gutiérrez, José María (2007). "Trends in Snakebite Envenomation Therapy: Scientific, Technological and Public Health Considerations". Current Pharmaceutical Design. 13 (28): 2935–50. doi:10.2174/138161207782023784. PMID 17979738.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b MedlinePlus - Snake bites From Tintinalli JE, Kelen GD, Stapcynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw Hill; 2004. Update Date: 2/27/2008. Updated by: Stephen C. Acosta, MD, Department of Emergency Medicine, Portland VA Medical Center, Portland, OR. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. Retrieved on 19 mars, 2009
- ^ Health-care-clinic.org - Snake Bite First Aid – Snakebite Retrieved on 21 mars, 2009
- ^ Snake bite image example at MDconsult - Patient Education - Wounds, Cuts and Punctures, First Aid for
- ^ Warrell, David A. (1976). "Snake Venom Ophthalmia and Blindness Caused by the Spitting Cobra (Naja Nigricollis) in Nigeria". The American Society of Tropical Medicine and Hygiene. 25 (3): 525–9. PMID 1084700. Retrieved 2009-09-05.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Ismail, Mohammad (1993). "The ocular effects of spitting cobras: I. The ringhals cobra (Hemachatus haemachatus) Venom-Induced corneal opacification syndrome". Clinical Toxicology. 31 (1): 31–41. doi:10.3109/15563659309000372. PMID 8433414.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Confronting the Neglected Problem of Snake Bite Envenoming: The Need for a Global Partnership". PLoS Medicine. Retrieved 2012-06-06.
- ^ a b Phillips, Charles M. (2002). "Sea snake envenomation" (PDF). Dermatologic Therapy. 15 (1): 58–61(4). doi:10.1046/j.1529-8019.2002.01504.x. Retrieved 2009-07-24.
- ^ a b Young, Bruce A. (2002). "Do Snakes Meter Venom?". BioScience. 52 (12): 1121–26. doi:10.1641/0006-3568(2002)052[1121:DSMV]2.0.CO;2.
The second major assumption that underlies venom metering is the snake's ability to accurately assess the target
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Young, Bruce A. (2001). "Venom flow in rattlesnakes: mechanics and metering" (PDF). Journal of Experimental Biology. 204 (Pt 24): 4345–4351. PMID 11815658.
With the species and size of target held constant, the duration of venom flow, maximum venom flow rate and total venom volume were all significantly lower in predatory than in defensive strikes
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Deufel, Alexandra (2003). "Feeding in Atractaspis (Serpentes: Atractaspididae): a study in conflicting functional constraints" (PDF). Zoology. 106 (1): 43–61. doi:10.1078/0944-2006-00088. PMID 16351890. Retrieved 2009-08-25.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)[dead link] - ^ a b Jackson, Kate (2003). "The evolution of venom-delivery systems in snakes" (PDF). Zoological Journal of the Linnean Society. 137 (3): 337–354. doi:10.1046/j.1096-3642.2003.00052.x. Retrieved 2009-07-25.
- ^ Fry, Bryan G. (2006). "Early evolution of the venom system in lizards and snakes" (PDF). Nature. 439 (7076): 584–8. doi:10.1038/nature04328. PMID 16292255. Retrieved 2009-09-18.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Russell, Findlay E. (1980). "Snake Venom Poisoning in the United States". Annual Review of Medicine. 31: 247–59. doi:10.1146/annurev.me.31.020180.001335. PMID 6994610.
- ^ Spawls, Stephen (1997). The Dangerous Snakes of Africa. Johannesburg: Southern Book Publishers. p. 192. ISBN 1-86812-575-0.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c "National geographic- KING COBRA".
They are fiercely aggressive when cornered (line 28–29)
Cite error: The named reference "NG" was defined multiple times with different content (see the help page). - ^ "National geographic-BLACK MAMBA".
when threatened, highly aggressive (line 2–3)
- ^ Kurecki B, Brownlee H (1987). "Venomous snakebites in the United States". Journal of Family Practice. 25 (4): 386–92. PMID 3655676.
- ^ Gold B, Barish R (1992). "Venomous snakebites. Current concepts in diagnosis, treatment, and management". Emerg Med Clin North Am. 10 (2): 249–67. PMID 1559468.
- ^ Suchard, JR (1999). "Envenomations by Rattlesnakes Thought to Be Dead". The New England Journal of Medicine. 340 (24): 1930. doi:10.1056/NEJM199906173402420. PMID 10375322.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Gold BS, Wingert WA (1994). "Snake venom poisoning in the United States: a review of therapeutic practice". South. Med. J. 87 (6): 579–89. doi:10.1097/00007611-199406000-00001. PMID 8202764.
- ^ Pathmeswaran A, Kasturiratne A, Fonseka M, Nandasena S, Lalloo D, de Silva H (2006). "Identifying the biting species in snakebite by clinical features: an epidemiological tool for community surveys". Trans R Soc Trop Med Hyg. 100 (9): 874–8. doi:10.1016/j.trstmh.2005.10.003. PMID 16412486.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Chris Thompson. "Treatment of Australian Snake Bites". Australian anaesthetists' website.[dead link]
- ^ "Indian National Snakebite Protocols 2007" (PDF). Indian National Snakebite Protocol Consultation Meeting, 2nd August 2007, Delhi. Retrieved 31 May 2012.
- ^ Currie, Bart J. (2008). "Effectiveness of pressure-immobilization first aid for snakebite requires further study". Emergency Medicine Australasia. 20 (3): 267–270(4). doi:10.1111/j.1742-6723.2008.01093.x. PMID 18549384.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Patrick Walker, J (2013 Jan). "Venomous bites and stings". Current problems in surgery. 50 (1): 9–44. PMID 23244230.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b American College of Medical, Toxicology (2011 Dec). "Pressure immobilization after North American Crotalinae snake envenomation". Journal of medical toxicology : official journal of the American College of Medical Toxicology. 7 (4): 322–3. PMID 22065370.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wall, C (2012 Sep). "British Military snake-bite guidelines: pressure immobilisation". Journal of the Royal Army Medical Corps. 158 (3): 194–8. PMID 23472565.
{{cite journal}}: Check date values in:|date=(help) - ^ White, Julian (November 1991). "Oxyuranus microlepidotus". Chemical Safety Information from Intergovernmental Organizations. Retrieved 24 July 2009.
Without appropriate antivenom treatment up to 75% of taipan bites will be fatal. Indeed, in the era prior to specific antivenom therapy, virtually no survivors of taipan bite were recorded.
- ^ a b Theakston RD (1997). "An objective approach to antivenom therapy and assessment of first-aid measures in snake bite" (PDF). Ann. Trop. Med. Parasitol. 91 (7): 857–65. doi:10.1080/00034989760626. PMID 9625943.
- ^ Amaral CF, Campolina D, Dias MB, Bueno CM, Rezende NA (1998). "Tourniquet ineffectiveness to reduce the severity of envenoming after Crotalus durissus snake bite in Belo Horizonte, Minas Gerais, Brazil". Toxicon. 36 (5): 805–8. doi:10.1016/S0041-0101(97)00132-3. PMID 9655642.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Watt G, Padre L, Tuazon ML, Theakston RD, Laughlin LW (1988). "Tourniquet application after cobra bite: delay in the onset of neurotoxicity and the dangers of sudden release". Am. J. Trop. Med. Hyg. 38 (3): 618–22. PMID 3275141.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Holstege CP, Singletary EM (2006). "Images in emergency medicine. Skin damage following application of suction device for snakebite". Annals of Emergency Medicine. 48 (1): 105, 113. doi:10.1016/j.annemergmed.2005.12.019. PMID 16781926.
- ^ Alberts M, Shalit M, LoGalbo F (2004). "Suction for venomous snakebite: a study of "mock venom" extraction in a human model". Ann Emerg Med. 43 (2): 181–6. doi:10.1016/S0196-0644(03)00813-8. PMID 14747805.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bush SP, Hegewald KG, Green SM, Cardwell MD, Hayes WK (2000). "Effects of a negative pressure venom extraction device (Extractor) on local tissue injury after artificial rattlesnake envenomation in a porcine model". Wilderness & environmental medicine. 11 (3): 180–8. doi:10.1580/1080-6032(2000)011[0180:EOANPV]2.3.CO;2. PMID 11055564.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Riggs BS, Smilkstein MJ, Kulig KW, et al. Rattlesnake envenomation with massive oropharyngeal edema following incision and suction (Abstract). Presented at the AACT/AAPCC/ABMT/CAPCC Annual Scientific Meeting, Vancouver, Canada, September 27 October 2, 1987.
- ^ Russell F (1987). "Another warning about electric shock for snakebite". Postgrad Med. 82 (5): 32. PMID 3671201.
- ^ Ryan A (1987). "Don't use electric shock for snakebite". Postgrad Med. 82 (2): 42. PMID 3497394.
- ^ Howe N, Meisenheimer J (1988). "Electric shock does not save snakebitten rats". Ann Emerg Med. 17 (3): 254–6. doi:10.1016/S0196-0644(88)80118-5. PMID 3257850.
- ^ Johnson E, Kardong K, Mackessy S (1987). "Electric shocks are ineffective in treatment of lethal effects of rattlesnake envenomation in mice". Toxicon. 25 (12): 1347–9. doi:10.1016/0041-0101(87)90013-4. PMID 3438923.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Russell, F. E. (1990). "When a snake strikes". Emerg Med. 22 (12): 33–4, 37–40, 43.
- ^ a b Mackessy, Stephen P. (2002). "Biochemistry and pharmacology of colubrid snake venoms" (PDF). Journal of Toxicology: Toxin Reviews. 21 (1–2): 43–83. doi:10.1081/TXR-120004741. Retrieved 2009-09-26.
Estimates of the number of venomous colubrids approach 700 species. Most may not produce a venom capable of causing serious damage to humans, but at least five species (Dispholidus typus, Thelotornis capensis, Rhabdophis tigrinus, Philodryas olfersii and Tachymenis peruviana) have caused human fatalities
- ^ a b Wingert W, Chan L (1 January 1988). "Rattlesnake Bites in Southern California and Rationale for Recommended Treatment". West J Med. 148 (1): 37–44. PMC 1026007. PMID 3277335.
- ^ Gutiérrez, José María (6 June 2006). "Confronting the Neglected Problem of Snake Bite Envenoming: The Need for a Global Partnership". PLOS Medicine. 3 (6): e150. doi:10.1371/journal.pmed.0030150. PMC 1472552. PMID 16729843. Retrieved 2009-06-30.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ^ Parrish H (1966). "Incidence of treated snakebites in the United States". Public Health Rep. 81 (3): 269–76. doi:10.2307/4592691. PMC 1919692. PMID 4956000.
- ^ a b White, Nancy (2009). Black Mambas: Sudden Death!. Bearport Publishing. ISBN 1597167665.
- ^ a b c Davidson, Terence. "IMMEDIATE FIRST AID". University of California, San Diego. Cite error: The named reference "Davidson" was defined multiple times with different content (see the help page).
- ^ Crisp, NG (31). "Black mamba envenomation". South African Medical Journal. 68 (5): 293–4. PMID 4035489.
{{cite journal}}:|access-date=requires|url=(help); Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ Hilligan, R (1). "Black mamba bites. A report of 2 cases". South African Medical Journal. 72 (3): 220–1. PMID 3603321. Retrieved 20 October 2013.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ a b "IMMEDIATE FIRST AID for bites by Australian taipan or common taipan".
- ^ "University of Adelaide Clinical Toxinology Resources".
Mortality rate:70-80%
- ^ "University of Adelaide Clinical Toxinology Resources".
Mortality rate:80%
- ^ "Australia's 10 most dangerous snakes". Australian Geographic. Australian Geographic. Retrieved 20 October 2013.
- ^ "Saw-scaled viper". Encyclopedia Britannica. Encyclopedia Britannica. Retrieved 20 October 2013.
- ^ "University of Adelaide Clinical Toxinology Resources".
- ^ "University of Adelaide Clinical Toxinology Resources".
Mortality rate:50-60%
- ^ "Australia's 10 most dangerous snakes". Australian Geographic. Australian Geographic. Retrieved 20 October 2013.
- ^ University of Adelaide Clinical Toxinology Resource
- ^ a b c Mallow D, Ludwig D, Nilson G. 2003. True Vipers: Natural History and Toxinology of Old World Vipers. Malabar, Florida: Krieger Publishing Company. 359 pp. ISBN 0-89464-877-2.
- ^ a b Brown JH. 1973. Toxicology and Pharmacology of Venoms from Poisonous Snakes. Springfield, Illinois: Charles C. Thomas. 184 pp. LCCCN 73-229. ISBN 0-398-02808-7. Cite error: The named reference "Bro73" was defined multiple times with different content (see the help page).
- ^ Spawls S, Branch B. 1995. The Dangerous Snakes of Africa. Ralph Curtis Books. Dubai: Oriental Press. 192 pp. ISBN 0-88359-029-8.
- ^ Engelmann, Wolf-Eberhard (1981). Snakes: Biology, Behavior, and Relationship to Man. Leipzig; English version NY, USA: Leipzig Publishing; English version published by Exeter Books (1982). p. 51. ISBN 0-89673-110-3.
- ^ Brown, John H. (1973). Toxicology and Pharmacology of Venoms from Poisonous Snakes. Springfield, IL USA: Charles C. Thomas. p. 81. ISBN 0-398-02808-7.
- ^ Clinical Toxinology Resource (Dendroaspis jamesoni)
- ^ Whitaker Z. 1990. Snakeman. Penguin Books Ltd. 192 pp. ISBN 0-14-014308-4.
- ^ a b University of Adelaide Clinical Toxinology Resource
- ^ Handbook of clinical toxicology of animal venoms and poisons. Vol. 236. USA: CRC Press. 1995. ISBN 0-8493-4489-1.
- ^ Greene, HW (1997). Snakes: The Evolution of Mystery in Nature. California, USA: University of California Press. ISBN 0520224876.
- ^ Tweedie, MWF (1983). The Snakes of Malaya. Singapore: Singapore National Printers Ltd. ISBN B0007B41IO.
{{cite book}}: Check|isbn=value: invalid character (help) - ^ Mathew, Gera, JL, T. "http://www.priory.com/med/ophitoxaemia.htm". MEDICINE ON-LINE. Retrieved 20 October 2013.
{{cite web}}: External link in|title= - ^ Stephen P. Mackessy: Biochemistry and Pharmacology of Colubrid Snake Venoms. J. Toxicol.—Toxin Reviews 21 (1&2), 2002: pp. 43–83 online PDF
- ^ a b Schneemann, M. (2004). "Life-threatening envenoming by the Saharan horned viper (Cerastes cerastes) causing micro-angiopathic haemolysis, coagulopathy and acute renal failure: clinical cases and review" (PDF). QJM: an International Journal of Medicine. 97 (11): 717–27. doi:10.1093/qjmed/hch118. PMID 15496528. Retrieved 2009-09-04.
This echoed the opinion of the Egyptian physicians who wrote the earliest known account of the treatment of snake bite, the Brooklyn Museum Papyri, dating perhaps from 2200 BC. They regarded bites by horned vipers 'fy' as non-lethal, as the victims could be saved.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c Anil, Aggrawal (2004). "Homicide with snakes: A distinct possibility and its medicolegal ramifications". Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology. 4 (2).
- ^ Crawford, Amy (April 1, 2007). "Who Was Cleopatra? Mythology, propaganda, Liz Taylor and the real Queen of the Nile". Smithsonian.com. Retrieved 4 September 2009.
- ^ Warrell, D.A. (2009). "Commissioned article: management of exotic snakebites". QJM: an International Journal of Medicine. 102 (9): 593–601. doi:10.1093/qjmed/hcp075. PMID 19535618.
- ^ Straight, Richard C. (1994). "Human fatalities caused by venomous animals in Utah, 1900–90". Great Basin Naturalist. 53 (4): 390–4. Retrieved 2009-09-04.
A third unusual death was a tragic fatality (1987), recorded as a homicide, which resulted when a large rattlesnake (G. v. lutosus) bit a 22-month-old girl after the snake had been placed around her neck (Washington County). The child died in approximately 5 h.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Strubel, T. (2008). "Suizidversuch durch Schlangenbiss: Kasuistik und Literaturübersicht". Der Nervenarzt (in German). 79 (5): 604–6. doi:10.1007/s00115-008-2431-4. PMID 18365165.
Ein etwa 20-jähriger Arbeiter wurde nach dem Biss seiner Puffotter (Bitis arietans) in die Hand auf die toxikologische Intensivstation aufgenommen. Zunächst berichtet der Patient, dass es beim „Melken" der Giftschlange zu dem Biss gekommen sei, erst im weiteren Verlauf räumt er einen Suizidversuch ein. Als Gründe werden Einsamkeit angeführt sowie unerträgliche Schmerzen im Penis.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)
- Bibliography
- Greene, Harry W. (1997). Snakes: The Evolution of Mystery in Nature. Berkeley, CA: University of California Press. ISBN 978-0-520-20014-2.
{{cite book}}: Invalid|ref=harv(help) - Stephen P., Mackessy, ed. (2010). Handbook of Venoms and Toxins of Reptiles (2nd ed.). Boca Raton, FL: CRC Press. ISBN 978-0-8493-9165-1.
{{cite book}}: Invalid|ref=harv(help) - Valenta, Jiri (2010). Venomous Snakes: Envenoming, Therapy (2nd ed.). Hauppauge, NY: Nova Science Publishers. ISBN 978-1-60876-618-5.
{{cite book}}: Invalid|ref=harv(help)
Further reading
- Campbell, Jonathan A.; William W. Lamar (2004). The Venomous Reptiles of the Western Hemisphere. Ithaca, NY: Cornell University Press. ISBN 978-0-8014-4141-7
- Spawls, Stephen; Bill Branch (1995). The Dangerous Snakes of Africa: Natural History, Species Directory, Venoms and Snakebite. Sanibel Island, FL: Ralph Curtis Publishing. ISBN 978-0-88359-029-4
- Sullivan JB, Wingert WA, Norris Jr RL. (1995). North American Venomous Reptile Bites. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. 3: 680–709.
- Thorpe, Roger S.; Wolfgang Wüster, Anita Malhotra (1996). Venomous Snakes: Ecology, Evolution, and Snakebite'. Oxford, England: Oxford University Press. ISBN 978-0-19-854986-4