- Home/
- Newsroom/
- Photo stories/
- item/
- Case study: Dengue in Portugal
Case study: Dengue in Portugal
“The mosquitoes are here. The mosquitoes are spreading.”
On entry to the insectary, steam billows out of the second protective door, fogging up glasses and camera lenses.
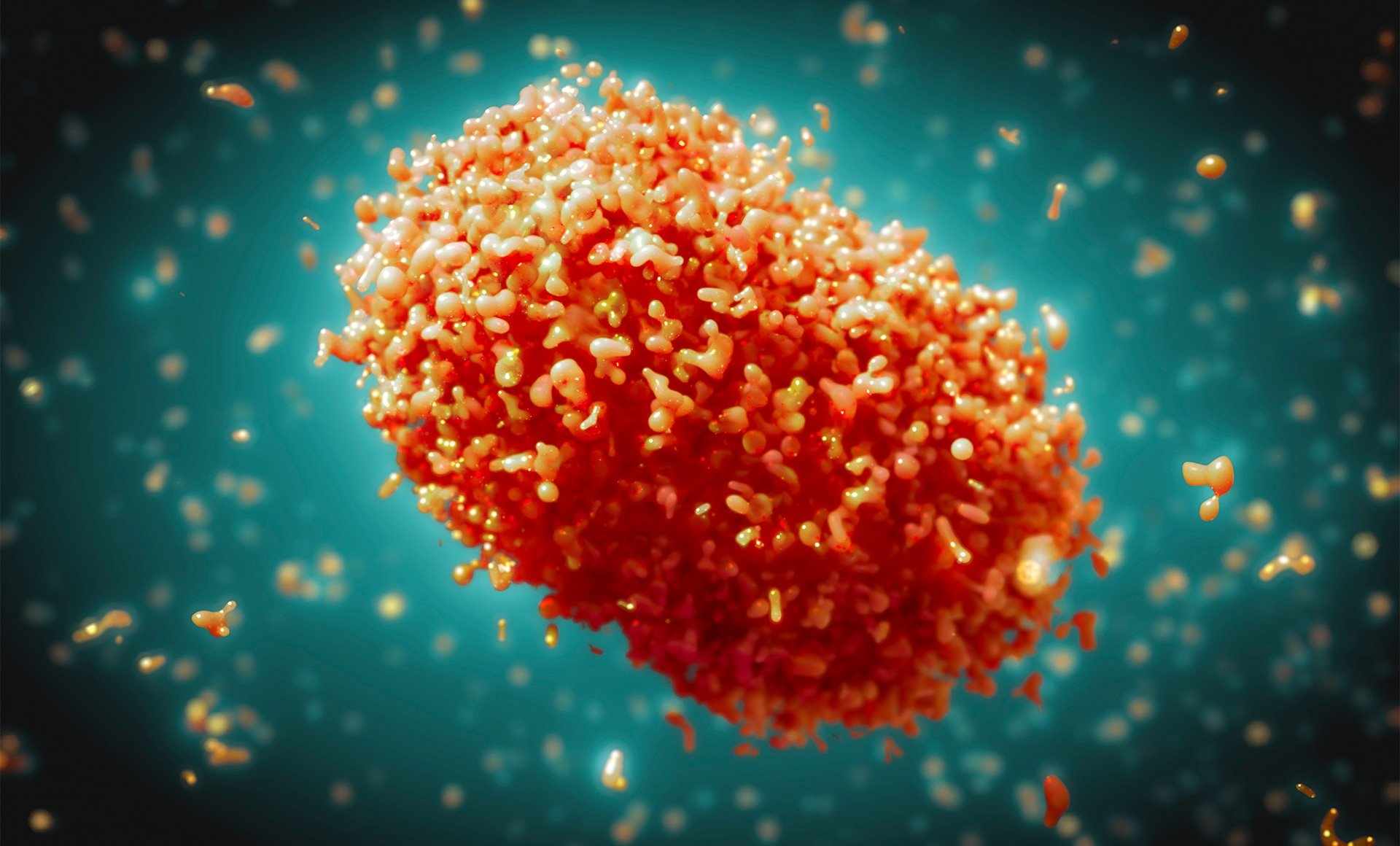
This room at the Instituto de Higiene e Medicina Tropical (IHMT) in Lisbon, Portugal, must be kept at the perfect conditions for mosquito larvae to thrive and grow into their adult form. As adults, they are infected with the dengue virus (DENV) within a biohazard facility in the same building. This allows the scientists to study their behaviour before dissecting and handing them to the virologists who examine their tiny cells under microscopes.
Research into the biological mechanisms of this disease could contribute to breakthrough treatment and vaccination to curb transmission among human populations – both in the WHO European Region and around the world.
Portugal is one of the countries in the Region identified by WHO to possess the climatic suitability for pathogens causing dengue to spread. Both mosquitoes that carry the DENV – Aedes aegypti and Aedes albopictus – reappeared in the 2000s through a combination of international travel and global trade, coupled with a changing climate that allows them to thrive.
Professor Carla Sousa leads dengue research at IHMT and explains that the eggs of Aedes albopictus, also known as the Asian Tiger mosquito, can be viable for several months even if they are completely dry.
This means they can survive extensive periods in hostile environments, a characteristic which makes them great travellers.
“It’s an emerging disease, and in the last couple of decades, the number of imported cases arriving to Portugal are increasing as well as in the other countries of Europe,” says Professor Sousa.
At present Aedes albopictus is the sole vector on the Portuguese mainland; Aedes aegypti has been detected only in Madeira, a Portuguese island, and was responsible for the outbreak in 2012, which resulted in over 2000 cases. This mosquito is a more “competent vector” – a much better transmitter of disease – and surveillance systems are in place to ensure health authorities are alerted if and when it reaches the mainland.
Madeira, however, has experienced so-called autochthonous cases, which occur when the disease is locally transmitted. This is more of a worry because it can lead to sporadic outbreaks. Professor Sousa and her wider team act as consultants for national (General Directorate of Health), regional (Health Secretary for the Madeira Autonomous Region), and international (WHO) health authorities to provide technical support during arboviral outbreaks or vector-based emergencies.
How can the threat of dengue be monitored and prevented?
It’s not only the scientists and surveillance networks that track mosquitoes. Mosquito Web is a citizen-science project set up by IHMT to encourage people to submit images of mosquitoes to an online platform. The photos are then analysed by experts to understand the epidemiological spread of mosquitoes across the country. These data can result in early detection of dengue vectors and, thanks to citizen involvement, the presence of Aedes albopictus was recorded for the first time in Lisbon.
Aedes mosquitoes in the field are persistent and aggressive. Simply not satisfied with one blood meal, they will follow people around their campsite, supermarket or street, and are able to feed many times in one sitting throughout the day, rather than only at dawn or dusk like other species. However, if the mosquitoes are not infected, this presents a nuisance rather than anything more serious.
Research into these vectors takes place in VIASEF, a specialist unit within IHMT NOVA. Mosquitoes are reared by insectary technician Ana Catarina Alves and it’s her job to keep the rooms at optimum temperature and humidity, while providing mosquitoes with their meals – sometimes blood, sometimes a glucose solution. Her work is clearly labour-intensive and time-consuming but feeds into research to understand the genomics of Aedes and their viral transmission. This could lead to vaccine candidates; integral to protect against dengue and other infectious diseases spread by the bite of a female mosquito.
Dr Marcelo Ferreira, Senior Investigator at IHMT
How is dengue diagnosed?
Dengue is complex and can lead to a variety of different symptoms. This makes it hard to diagnose and especially difficult when compared to other illnesses causing fever and flu-like symptoms. Dr Marcelo Ferreira, Senior Investigator at IHMT, explains that 60–70% of cases are asymptomatic, adding another layer of complication.
“Doctors, even in health centres, will see very few cases,” says Dr Ferreira. “The problem with dengue is the number of confirmed cases is still small. And that's why people don't think about it. Even among the symptomatic cases, most people will have relatively unspecific illness – so, fever, headache, some other aches and pains in the body but nothing very typical of dengue. That's again why prior suspicion is very important.”
Most cases of dengue fever are seen in the Lisbon travel medicine clinic where the patient has a history of travel to a region where dengue is endemic and are aware they may have caught the disease.
When there are outbreaks in other parts of the world, this impacts the likelihood of imported cases, especially countries such as Brazil and Mozambique, where Portuguese residents may be visiting family and friends.
When a patient is diagnosed with dengue, or suspected dengue, doctors treat first and foremost with pain medication to alleviate symptoms, such as headaches, joint pain, and high fever, since there is no specific medication for this disease. Pain relief helps ease the symptoms and, generally, patients make a full recovery.
Nevertheless, as Dr Ferreira cautions, the second time a person catches dengue it may lead to more severe symptoms and a more serious manifestation of the disease. Dengue has 4 serotypes – essentially 4 different viruses named DENV 1, DENV 2, DENV 3 and DENV 4. If someone catches dengue for the first time, they will build immunity to one of the viruses but catching dengue a second time could lead to severe dengue haemorrhagic fever. Severe dengue, dengue haemorrhagic fever or dengue shock syndrome happens when one’s blood vessels become damaged and leaky. This can lead to shock, internal bleeding, organ failure and even death.
What does this mean for the Region?
This situation poses a major public health challenge. WHO has determined that the threat is high worldwide, considering the growing risk of transmission and the increase in cases and deaths.
Climate change is already affecting the distribution and seasonality of the mosquito vectors and climatic conditions conducive to virus transmission. Among the 30 countries identified by WHO as suitable for dengue transmission – mainly along the Mediterranean coast – France, Italy, and Spain have already experienced locally acquired cases of dengue fever.
Enhanced surveillance of dengue is in place in these areas, especially during the mosquito season in the summer. This is crucial for early detection and appropriate disease control measures.
To protect yourself, preventing mosquito bites is the best way to avoid getting dengue. It is important to be vigilant in the daytime, as this is when Aedes are most likely to feed. Using mosquito repellent and wearing long-sleeved clothes can help to deter mosquitoes.