- News
- City News
- delhi News
- Delivered! Happy result after seven failed pregnancies
Trending
Delivered! Happy result after seven failed pregnancies
A woman from Haryana gave birth at AIIMS after receiving O D -- phenotype red cell units from Japan for her eighth successful pregnancy, overcoming HDFN. This rare procedure is the first in India and eighth globally.

Representativd Image
NEW DELHI: After facing seven failed pregnancies, a young woman from Haryana in her twenties recently gave birth to a healthy girl at AIIMS. This was made possible by the successful transfusion of O D -- phenotype red cell units obtained from Japan to help the fetus survive. The procedure is said to be the first of its kind in India and the eighth successful one in the world.
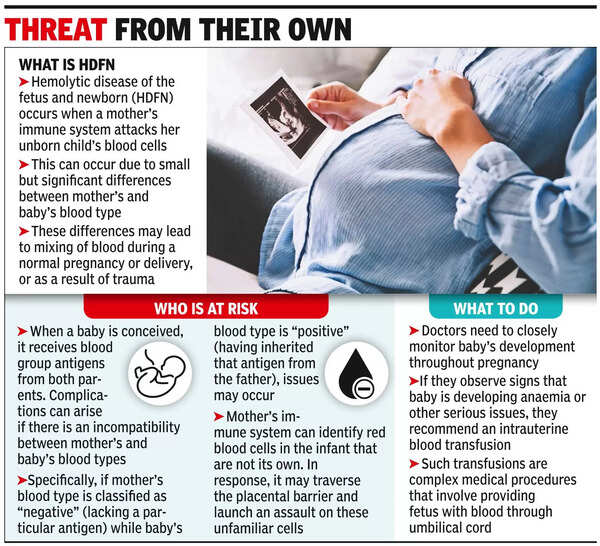
These specialised blood units were used for intrauterine transfusion, a procedure that helped ensure the health and survival of the unborn child suffering from severe anaemia due to haemolysis (destruction of red blood cells) caused by antibodies transferred from the mother. This condition is called haemolytic disease of the fetus and newborn (HDFN).

HDFN is a significant cause of fetal morbidity and mortality in the antenatal period and immediate postnatal period, said doctors. This case study was published recently in PubMed.
According to doctors, intrauterine transfusion involves the injection of donor red blood cells directly into the fetus. Two common causes of
Dr K Aparna Sharma of the obstetrics and gynaecology department at AIIMS explained that Rh incompatibility arose when the mother and fetus had differing blood types. In this particular case, the mother's blood contained anti-RH17 antibodies, which attacked and destroyed the fetal blood cells. This led to a severe decrease in the fetus' red blood cell count, necessitating an intrauterine transfusion to prevent further complications.
Since there is no rare donor registry in India, the International Rare Donor Panel was contacted to arrange O D -- phenotype red cell units. Though a blood donor from India was registered on the panel, he refused to make a donation.
"To ensure the safety and well-being of the fetus, we reached out to the Japanese Red Cross, which has a registry of 32 donors with the rare O D -- blood type. It agreed to transport the blood,” said Dr Vatsal Dadhwal. “To save the fetus throughout the pregnancy, three units of O D -- red blood cells were sent from the Japanese Red Cross to our facility at intervals, specifically for the purpose of intrauterine transfusion."
According to the head of the obstetrics and gynaecology department, Dr Neena Malhotra, there have been just 18 cases globally of Rh– pregnancy with anti-Rh17 reported. Out of these, only eight pregnancies had successful outcomes. This was the first successful case in India.
Dr Anubhuti Rana, also of the obstetrics and gynaecology department, disclosed the expenses related to the blood transportation was Rs 4,10,596. The cost was covered by two NGOs on separate occasions. “Rs 1.37 lakh was given by Relaxo and Rs 1.37 lakh by Sai Trust," she said. Additionally, Rastriya Arogya Nidhi contributed Rs 1,36,590 for the transportation in the third instance.
Rana added that fetal therapy was offered in a few centres in the country and the department at AIIMS was one of the leading centres among them. However, timely referral was crucial to save the life of the baby.
Dr Hemchand Pandey of the department of transfusion medicine also deserved recognition for pinpointing the issue at hand. The successful identification of the problem was the key advantage in this particular case.
These specialised blood units were used for intrauterine transfusion, a procedure that helped ensure the health and survival of the unborn child suffering from severe anaemia due to haemolysis (destruction of red blood cells) caused by antibodies transferred from the mother. This condition is called haemolytic disease of the fetus and newborn (HDFN).
HDFN is a significant cause of fetal morbidity and mortality in the antenatal period and immediate postnatal period, said doctors. This case study was published recently in PubMed.
The woman's case marks the first successful pregnancy of its kind in India, where the use of internationally sourced O D -- phenotype red cell units played a crucial role in overcoming the challenges posed by her previous unsuccessful attempts at childbirth. All her pregnancies were earlier managed at primary or secondary-level centres and she never received a blood transfusion.
According to doctors, intrauterine transfusion involves the injection of donor red blood cells directly into the fetus. Two common causes of
fetal anaemia are Rh incompatibility and maternal Parvovirus B19 viral infection.
Dr K Aparna Sharma of the obstetrics and gynaecology department at AIIMS explained that Rh incompatibility arose when the mother and fetus had differing blood types. In this particular case, the mother's blood contained anti-RH17 antibodies, which attacked and destroyed the fetal blood cells. This led to a severe decrease in the fetus' red blood cell count, necessitating an intrauterine transfusion to prevent further complications.
Since there is no rare donor registry in India, the International Rare Donor Panel was contacted to arrange O D -- phenotype red cell units. Though a blood donor from India was registered on the panel, he refused to make a donation.
"To ensure the safety and well-being of the fetus, we reached out to the Japanese Red Cross, which has a registry of 32 donors with the rare O D -- blood type. It agreed to transport the blood,” said Dr Vatsal Dadhwal. “To save the fetus throughout the pregnancy, three units of O D -- red blood cells were sent from the Japanese Red Cross to our facility at intervals, specifically for the purpose of intrauterine transfusion."
According to the head of the obstetrics and gynaecology department, Dr Neena Malhotra, there have been just 18 cases globally of Rh– pregnancy with anti-Rh17 reported. Out of these, only eight pregnancies had successful outcomes. This was the first successful case in India.
Dr Anubhuti Rana, also of the obstetrics and gynaecology department, disclosed the expenses related to the blood transportation was Rs 4,10,596. The cost was covered by two NGOs on separate occasions. “Rs 1.37 lakh was given by Relaxo and Rs 1.37 lakh by Sai Trust," she said. Additionally, Rastriya Arogya Nidhi contributed Rs 1,36,590 for the transportation in the third instance.
Rana added that fetal therapy was offered in a few centres in the country and the department at AIIMS was one of the leading centres among them. However, timely referral was crucial to save the life of the baby.
Dr Hemchand Pandey of the department of transfusion medicine also deserved recognition for pinpointing the issue at hand. The successful identification of the problem was the key advantage in this particular case.
End of Article
FOLLOW US ON SOCIAL MEDIA