Background and Overview
Despite the widespread availability and use of potent antiretroviral therapy, individuals with HIV continue to suffer significant morbidity and mortality from opportunistic infections, defined as infections that are more frequent or severe due to immunosuppression. The introduction of effective antiretroviral therapy in the mid-1990s led to a dramatic decline in the rate of AIDS-defining opportunistic infections in the United States (Figure 1), and these declines involved all major AIDS-defining opportunistic infections (Figure 2).[1,2] During 2000 through 2010 (in the United States and Canada), AIDS-defining opportunistic infections occurred at a low rate and there were further declines during this decade (Figure 3).[3] In the current era, the rate of AIDS-defining opportunistic infections has remained low. Nevertheless, these opportunistic infections can still occur in individuals with HIV, particularly in the setting of undiagnosed HIV, late diagnosis of HIV, or in persons with known HIV who are not engaged in care. Clinicians who provide care to persons with HIV should have basic competency in the prevention, diagnosis, and treatment of common AIDS-defining opportunistic infections. This Topic Review provides an overview of the prophylaxis of the most common and important opportunistic infections that occur in persons with HIV. The content is based on recommendations in the Adult and Adolescent OI Guidelines.[4]
 Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy
Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza
Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Dolutegravir-Abacavir-Lamivudine Triumeq
Dolutegravir-Abacavir-Lamivudine Triumeq Dolutegravir-Lamivudine Dovato
Dolutegravir-Lamivudine Dovato Dolutegravir-Rilpivirine Juluca
Dolutegravir-Rilpivirine Juluca Doravirine-Tenofovir DF-Lamivudine Delstrigo
Doravirine-Tenofovir DF-Lamivudine Delstrigo Efavirenz-Tenofovir DF-Emtricitabine Atripla
Efavirenz-Tenofovir DF-Emtricitabine Atripla Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya
Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild
Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey
Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey Rilpivirine-Tenofovir DF-Emtricitabine Complera
Rilpivirine-Tenofovir DF-Emtricitabine Complera Enfuvirtide Fuzeon
Enfuvirtide Fuzeon Fostemsavir Rukobia
Fostemsavir Rukobia Ibalizumab Trogarzo
Ibalizumab Trogarzo Maraviroc Selzentry
Maraviroc Selzentry Dolutegravir Tivicay
Dolutegravir Tivicay Raltegravir Isentress
Raltegravir Isentress Abacavir Ziagen
Abacavir Ziagen Abacavir-Lamivudine Epzicom
Abacavir-Lamivudine Epzicom Abacavir-Lamivudine-Zidovudine Trizivir
Abacavir-Lamivudine-Zidovudine Trizivir Didanosine Videx
Didanosine Videx Emtricitabine Emtriva
Emtricitabine Emtriva Lamivudine Epivir
Lamivudine Epivir Stavudine Zerit
Stavudine Zerit Tenofovir alafenamide-Emtricitabine Descovy
Tenofovir alafenamide-Emtricitabine Descovy Tenofovir DF Viread
Tenofovir DF Viread Tenofovir DF-Emtricitabine Truvada and Multiple Generics
Tenofovir DF-Emtricitabine Truvada and Multiple Generics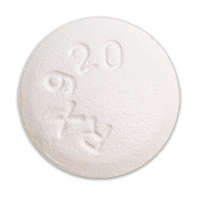 Zidovudine Retrovir
Zidovudine Retrovir Zidovudine-Lamivudine Combivir
Zidovudine-Lamivudine Combivir Doravirine Pifeltro
Doravirine Pifeltro Efavirenz Sustiva
Efavirenz Sustiva Etravirine Intelence
Etravirine Intelence Nevirapine Viramune
Nevirapine Viramune Rilpivirine Edurant
Rilpivirine Edurant Atazanavir Reyataz
Atazanavir Reyataz Atazanavir-Cobicistat Evotaz
Atazanavir-Cobicistat Evotaz Darunavir Prezista
Darunavir Prezista Darunavir-Cobicistat Prezcobix
Darunavir-Cobicistat Prezcobix Fosamprenavir Lexiva
Fosamprenavir Lexiva Indinavir Crixivan
Indinavir Crixivan Lopinavir-Ritonavir Kaletra
Lopinavir-Ritonavir Kaletra Nelfinavir Viracept
Nelfinavir Viracept Saquinavir Invirase
Saquinavir Invirase Tipranavir Aptivus
Tipranavir Aptivus Cobicistat Tybost
Cobicistat Tybost Ritonavir Norvir
Ritonavir Norvir








