Background
The United States correctional system consists of local and tribal jails, state prisons, federal prisons, military and immigration facilities, and community correctional facilities, which include probation and parole programs.[1]
- Jails: Typically, jails house persons charged with a crime who are awaiting trial or transfer, as well as persons convicted who have sentences of less than 1 or 2 years. Persons leaving jail are often supervised on probation for a defined period of time.
- Prisons: In contrast to jails, prisons house persons convicted of a felony serving longer sentences. Whether the offense committed involves federal law or state law determines placement in a federal or state prison.
- Parole: The term parole refers to conditional release from prison prior to completing a sentence with the responsibility of completing the remainder of the sentence in the community. Upon leaving prison, many people continue to be monitored by the correctional system while on parole.
At any point in time, about twice as many persons are incarcerated in prisons than in jails in the United States, but over the course of a year the number of individuals incarcerated in the jail system far exceeds those incarcerated in prisons (Figure 1); this difference over a year results from the low turnover rates in prisons (longer stays and infrequent releases) versus high turnover rates in jails (shorter stays and frequent releases).[2]
Global Prison Statistics
In 2021, the United States had a higher total prison population in than any other country in the world (Figure 2).[3,4]
 Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy
Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza
Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Dolutegravir-Abacavir-Lamivudine Triumeq
Dolutegravir-Abacavir-Lamivudine Triumeq Dolutegravir-Lamivudine Dovato
Dolutegravir-Lamivudine Dovato Dolutegravir-Rilpivirine Juluca
Dolutegravir-Rilpivirine Juluca Doravirine-Tenofovir DF-Lamivudine Delstrigo
Doravirine-Tenofovir DF-Lamivudine Delstrigo Efavirenz-Tenofovir DF-Emtricitabine Atripla
Efavirenz-Tenofovir DF-Emtricitabine Atripla Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya
Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild
Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey
Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey Rilpivirine-Tenofovir DF-Emtricitabine Complera
Rilpivirine-Tenofovir DF-Emtricitabine Complera Enfuvirtide Fuzeon
Enfuvirtide Fuzeon Fostemsavir Rukobia
Fostemsavir Rukobia Ibalizumab Trogarzo
Ibalizumab Trogarzo Maraviroc Selzentry
Maraviroc Selzentry Dolutegravir Tivicay
Dolutegravir Tivicay Raltegravir Isentress
Raltegravir Isentress Abacavir Ziagen
Abacavir Ziagen Abacavir-Lamivudine Epzicom
Abacavir-Lamivudine Epzicom Abacavir-Lamivudine-Zidovudine Trizivir
Abacavir-Lamivudine-Zidovudine Trizivir Didanosine Videx
Didanosine Videx Emtricitabine Emtriva
Emtricitabine Emtriva Lamivudine Epivir
Lamivudine Epivir Stavudine Zerit
Stavudine Zerit Tenofovir alafenamide-Emtricitabine Descovy
Tenofovir alafenamide-Emtricitabine Descovy Tenofovir DF Viread
Tenofovir DF Viread Tenofovir DF-Emtricitabine Truvada and Multiple Generics
Tenofovir DF-Emtricitabine Truvada and Multiple Generics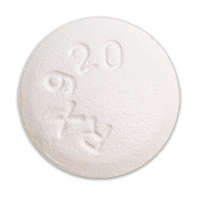 Zidovudine Retrovir
Zidovudine Retrovir Zidovudine-Lamivudine Combivir
Zidovudine-Lamivudine Combivir Doravirine Pifeltro
Doravirine Pifeltro Efavirenz Sustiva
Efavirenz Sustiva Etravirine Intelence
Etravirine Intelence Nevirapine Viramune
Nevirapine Viramune Rilpivirine Edurant
Rilpivirine Edurant Atazanavir Reyataz
Atazanavir Reyataz Atazanavir-Cobicistat Evotaz
Atazanavir-Cobicistat Evotaz Darunavir Prezista
Darunavir Prezista Darunavir-Cobicistat Prezcobix
Darunavir-Cobicistat Prezcobix Fosamprenavir Lexiva
Fosamprenavir Lexiva Indinavir Crixivan
Indinavir Crixivan Lopinavir-Ritonavir Kaletra
Lopinavir-Ritonavir Kaletra Nelfinavir Viracept
Nelfinavir Viracept Saquinavir Invirase
Saquinavir Invirase Tipranavir Aptivus
Tipranavir Aptivus Cobicistat Tybost
Cobicistat Tybost Ritonavir Norvir
Ritonavir Norvir







