Background
In the United States, the HIV epidemic disproportionately impacts racial and ethnic minority populations.[1] For all persons with HIV, accessible, affordable, and effective antiretroviral therapy is critical for improving health and preventing transmission of HIV. In the United States, since 2010, national strategies and priorities for HIV have emphasized reducing HIV-related health disparities and inequities, as well as ensuring that all persons with HIV receive access to treatment and care that is nonstigmatizing, culturally sensitive, and culturally competent.[2,3] Unfortunately, disparities and inequities continue to exist.
Clinician Awareness of HIV-Related Disparities
Multiple factors contribute to HIV-related disparities in the United States, including historical trauma, cultural differences, and socioeconomic inequalities. Clinicians working in the HIV field should be aware of these health disparities because they significantly impact clinical care. It is important to note that the racial disparities in HIV stem from long-standing and ongoing institutionalized racism and other sociostructural barriers, not biological differences. This Topic Review will address the epidemiology of HIV within racial and ethnic minority communities, highlight differences in engagement in care and HIV outcomes, explore key paradigms for understanding unique vulnerabilities to HIV among certain subpopulations, and investigate strategies to reduce HIV-related inequities in racial and ethnic minority populations.
 Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy
Bictegravir-Tenofovir alafenamide-Emtricitabine Biktarvy Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza
Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Dolutegravir-Abacavir-Lamivudine Triumeq
Dolutegravir-Abacavir-Lamivudine Triumeq Dolutegravir-Lamivudine Dovato
Dolutegravir-Lamivudine Dovato Dolutegravir-Rilpivirine Juluca
Dolutegravir-Rilpivirine Juluca Doravirine-Tenofovir DF-Lamivudine Delstrigo
Doravirine-Tenofovir DF-Lamivudine Delstrigo Efavirenz-Tenofovir DF-Emtricitabine Atripla
Efavirenz-Tenofovir DF-Emtricitabine Atripla Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya
Elvitegravir-Cobicistat-Tenofovir alafenamide-Emtricitabine Genvoya Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild
Elvitegravir-Cobicistat-Tenofovir DF-Emtricitabine Stribild Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey
Rilpivirine-Tenofovir alafenamide-Emtricitabine Odefsey Rilpivirine-Tenofovir DF-Emtricitabine Complera
Rilpivirine-Tenofovir DF-Emtricitabine Complera Enfuvirtide Fuzeon
Enfuvirtide Fuzeon Fostemsavir Rukobia
Fostemsavir Rukobia Ibalizumab Trogarzo
Ibalizumab Trogarzo Maraviroc Selzentry
Maraviroc Selzentry Dolutegravir Tivicay
Dolutegravir Tivicay Raltegravir Isentress
Raltegravir Isentress Abacavir Ziagen
Abacavir Ziagen Abacavir-Lamivudine Epzicom
Abacavir-Lamivudine Epzicom Abacavir-Lamivudine-Zidovudine Trizivir
Abacavir-Lamivudine-Zidovudine Trizivir Didanosine Videx
Didanosine Videx Emtricitabine Emtriva
Emtricitabine Emtriva Lamivudine Epivir
Lamivudine Epivir Stavudine Zerit
Stavudine Zerit Tenofovir alafenamide-Emtricitabine Descovy
Tenofovir alafenamide-Emtricitabine Descovy Tenofovir DF Viread
Tenofovir DF Viread Tenofovir DF-Emtricitabine Truvada and Multiple Generics
Tenofovir DF-Emtricitabine Truvada and Multiple Generics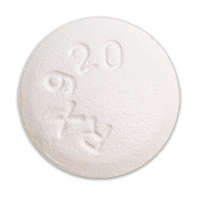 Zidovudine Retrovir
Zidovudine Retrovir Zidovudine-Lamivudine Combivir
Zidovudine-Lamivudine Combivir Doravirine Pifeltro
Doravirine Pifeltro Efavirenz Sustiva
Efavirenz Sustiva Etravirine Intelence
Etravirine Intelence Nevirapine Viramune
Nevirapine Viramune Rilpivirine Edurant
Rilpivirine Edurant Atazanavir Reyataz
Atazanavir Reyataz Atazanavir-Cobicistat Evotaz
Atazanavir-Cobicistat Evotaz Darunavir Prezista
Darunavir Prezista Darunavir-Cobicistat Prezcobix
Darunavir-Cobicistat Prezcobix Fosamprenavir Lexiva
Fosamprenavir Lexiva Indinavir Crixivan
Indinavir Crixivan Lopinavir-Ritonavir Kaletra
Lopinavir-Ritonavir Kaletra Nelfinavir Viracept
Nelfinavir Viracept Saquinavir Invirase
Saquinavir Invirase Tipranavir Aptivus
Tipranavir Aptivus Cobicistat Tybost
Cobicistat Tybost Ritonavir Norvir
Ritonavir Norvir







